The community had a meningitis problem. When kids were brought into a referral hospital in Cape Town, South Africa, with a suspected clinical case of meningitis, the only way to diagnose them was to do a lumbar puncture and test their spinal fluid.
The puncture was excruciating for kids—but it could save their lives. Meningitis can be fatal if left improperly diagnosed.
The problem was that too many laboratory tests came back inconclusive. The doctors couldn’t tell whether cases were bacterial or viral, which delayed proper treatment. In fact, out of more than 3,000 lumbar punctures performed at that hospital annually, only one percent of samples came back positive for bacterial meningitis.
Kids weren’t getting the antibiotics they needed in time.
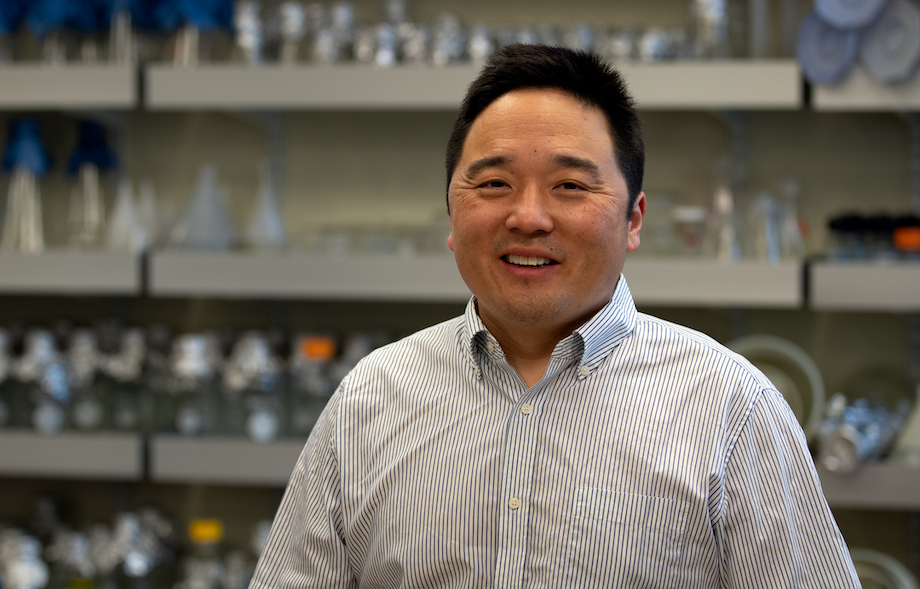
Jermaine Khumalo, Ph.D., was a master’s student at the University of Cape Town when he saw these puzzling results from the nearby hospital. Dr. Khumalo’s job was to re-run these samples and help devise a faster and more accurate way to test spinal fluid.
“I needed to come up with a real-time diagnostic tool that could distinguish between the major common causes of meningitis in children,” says Dr. Khumalo.
His PCR test (which detected genetic material from six possible pathogens) proved accurate and practical for use in a hospital setting. His analysis also showed doctors had missed another 30 percent of viral meningitis cases and five percent of bacterial meningitis cases in that initial group of patients. Tragically, some of those overlooked children had died.
“They died because they couldn’t get conclusive results,” says Dr. Khumalo. “That spurred on my work. I saw that if one improves diagnosis, one can improve therapy and save lives.”
Dr. Khumalo hadn’t set out to become an immunologist. As a kid in the newly independent country of Zimbabwe, he hadn’t known being a scientist was even a career option. The adults he knew were becoming lawyers, accountants, or medical doctors, so he thought he’d train as a physician as well. “I was always fascinated with the human body and biology as a whole,” he says.
As an undergraduate at Zimbabwe’s National University of Science and Technology, he realized life as a doctor wasn’t for him after a professor warned him of the grisly scenes he would encounter in a hospital. “That kind of trauma wasn’t for me,” says Dr. Khumalo.
Instead, Dr. Khumalo focused on saving lives through clinical research. “As an undergraduate, one of my favorite lecturers always talked about ‘demystifying’ immunology,” he says. “That was contagious, and I fell in love with the aspect of solving problems and finding things out.”
Working through the meningitis problem showed Dr. Khumalo the impact his work could have, so he set out to learn a lot more about how the immune system responds to disease.
“I looked for a lab that was attempting to uncover causes of disease pathogenesis,” says Dr. Khumalo. He ended up pursuing his Ph.D. in a University of Cape Town laboratory focused on tuberculosis and allergy research.
Allergy research presented another puzzle for Dr. Khumalo. In an allergic reaction, the body’s immune system overreacts to the molecules in an allergen, like dust mites or pollen. Immune cells go on the warpath, activating inflammatory molecules and wrecking healthy tissues. “That fascinated me,” he says. “How could the body mount this highly pathogenic immune and disruptive immune response against something harmless?”
“How could the body mount this highly pathogenic immune and disruptive immune response against something harmless?”
Jermaine Khumalo, Ph.D.
This work led to a passion for studying asthma. Asthma is a tough nut to crack because it looks different in almost every patient. The disease is driven by different allergens and can cause wheezing—or even death.
Dr. Khumalo’s graduate research revealed specific cell types important in asthma and clues to which treatments might work best in different patients. Still, Dr. Khumalo saw a problem. His work in mouse models showed a segment of mice resistant to treatment, just like many humans with severe asthma.
“Fifty percent of people with asthma respond perfectly to corticosteroid treatment, but there is a significant portion who don’t respond,” says Dr. Khumalo. Similar to meningitis, patients with asthma can die without good medications. “There are 300 million people affected by asthma in the world, and about half a million die every year from severe forms of the disease.”
Dr. Khumalo’s interest in these individual differences in asthma patients led him to apply for a postdoctoral position in the Vijayanand Lab at La Jolla Institute for Immunology (LJI).
Led by LJI Professor Pandurangan Vijayanand, M.D., Ph.D., the lab has pioneered the use of a technique called single-cell gene expression profiling. By looking at genetic expression in immune cells, the researchers can investigate how different human immune cells operate in diseases such as asthma.
Dr. Khumalo is studying samples from patients with and without severe asthma. This broad patient group is key, since Dr. Khumalo knows that any immune cell could hold important clues. No patient, no immune signature, is overlooked. “With high-throughput, single-cell sequencing, we are then able to isolate the responsible cells,” says Dr. Khumalo. This research has led him to focus on T cells, which can drive inflammation.
Dr. Khumalo’s work doesn’t stop there. In 2020, Khumalo was named an Intersect Fellow by the American Association of Immunologists and won support to pursue interdisciplinary research in a second LJI lab. In collaboration with the laboratory of LJI Associate Professor Ferhat Ay, Ph.D., Dr. Khumalo uses his skills in bioinformatics to analyze his immune cell data to find any disease-specific biomarkers.
By looking at asthma from every angle—through new patient groups, animal models, genetic factors, immune cell interactions, and environmental triggers—Dr. Khumalo hopes to spot what other researchers have missed. His end goal is to track down new drug targets for treating the disease.
“Once you solve a problem, you need to move on to the next one,” says Dr. Khumalo. “And it’s always exciting, even if an experiment fails. You fail and get back up, fail and get back up. But then an experiment finally works and you buy a bottle of wine.”
What is single-cell gene expression profiling?
Your cells all have nearly the same DNA code, but they don’t do the same jobs. For example, cells called nociceptors help sense pain, while beta cells in your pancreas make insulin. Your cells play their different roles thanks to changes in gene expression. This means a cell only “reads” a subset of genes to make certain proteins.
Immune cells do the same thing—that’s why there are so many different flavors of immune cells. For example, macrophages and T cells both fight pathogens, but they use different strategies, thanks to differences in their gene expression.
With single-cell gene expression profiling, scientists can discover exactly which genes are being expressed by individual immune cells in a sample. They can also figure out how gene expression changes, on a cell-by-cell basis, as they fight disease. This cutting-edge method is changing the field of immunology.
Using single-cell gene expression profiling, scientists in LJI’s Vijayanand Lab have uncovered new subsets of immune cells with jobs no one had ever witnessed before. In Dr. Khumalo’s research, single-cell gene expression profiling can reveal which immune cells overreact in cases of asthma—and how these haywire immune cells communicate with each other.