How sex-based differences shape the immune system—and what these discoveries mean for the future of medicine
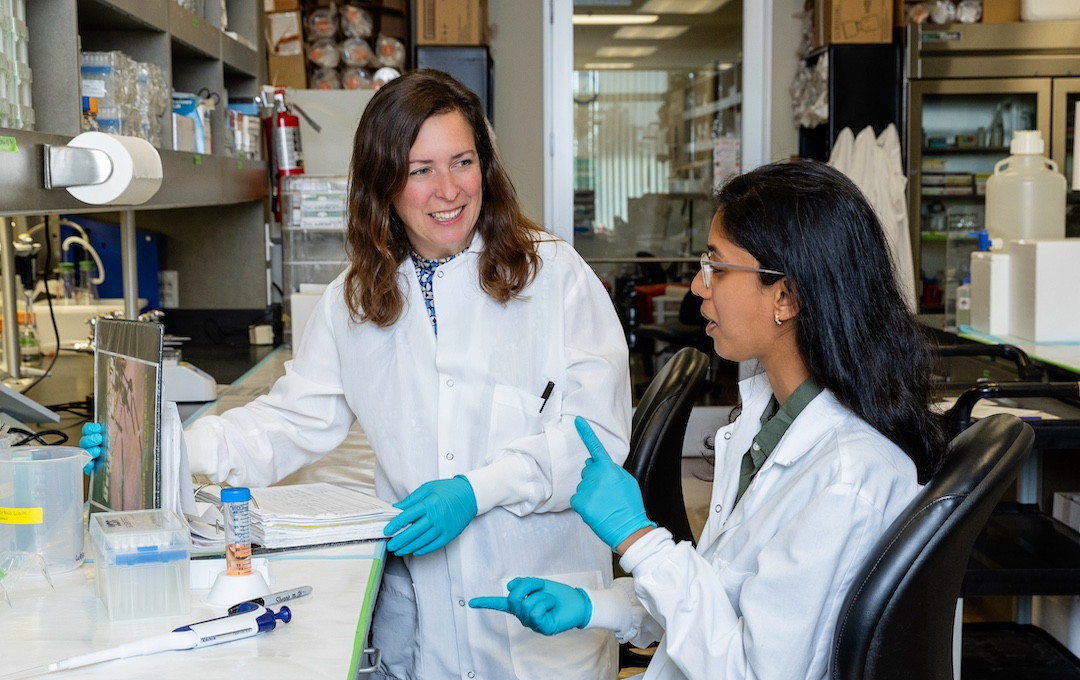
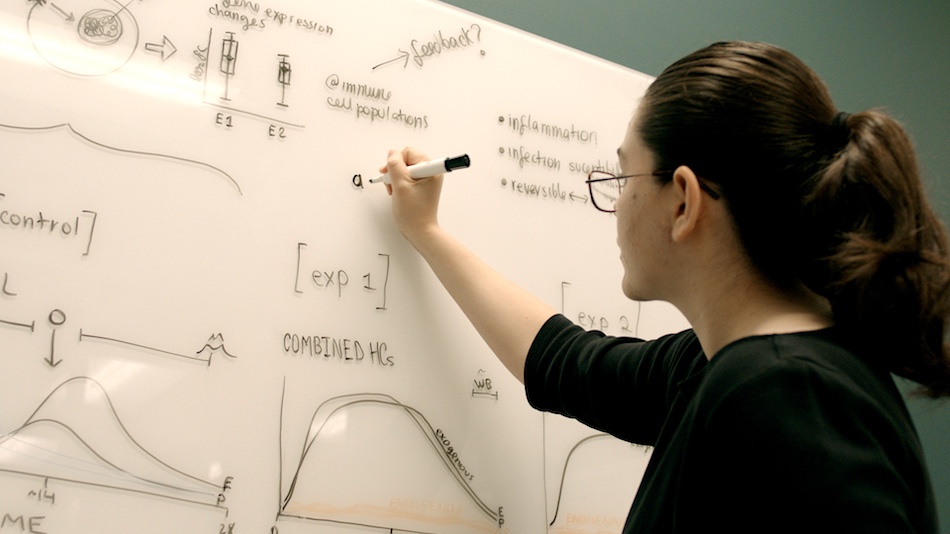
Just four years ago, scientists at La Jolla Institute for Immunology (LJI) launched the Center for Sex-Based Differences in the Immune System. This research hub brought together LJI scientists, collaborators, and supporters with a common goal: to investigate differences in how men’s and women’s bodies fight disease.
LJI Associate Professor Sonia Sharma, Ph.D., who is director of the Center, says this effort has revealed “profound” differences between male and female immune systems. The scientific community is now poised to translate those findings into clinical treatments.
“If we’re going to talk about ‘precision,’ or personal medicine at all, sex-based differences play a central role,” says Dr. Sharma. “Right now, we’re seeing an acceleration in sex-based-differences work, not only in academic research, but in the biotech field as well.”
LJI scientists are leading this new era of sex-based-differences research. Scientists across the Institute are taking the next step in figuring out how to harness these differences to treat autoimmune disease, strengthen cancer therapies, and protect all of us from pathogens.
How men and women fight viruses
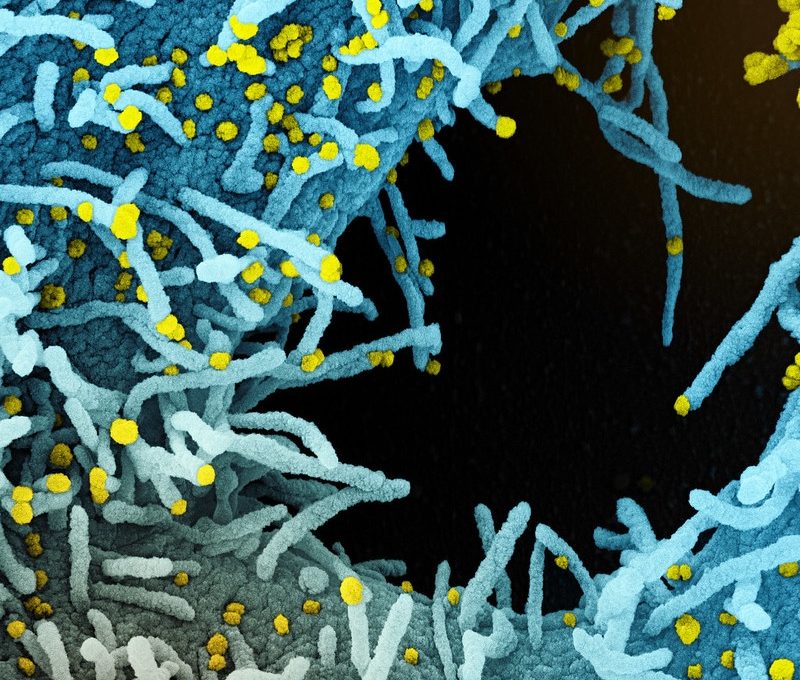
Why do more men suffer from severe COVID-19? Dr. Sharma’s own research may help solve this mystery. Her laboratory has found an enzyme that inhibits the body’s ability to fight SARS-CoV-2, the virus that causes COVID-19. Patients with XY chromosomes tend to have higher levels of this enzyme—which might be a big problem when SARS-CoV-2 attacks.
Learn more:
COVID-19 causes more severe disease in men. This tricky enzyme may be partially to blame.
Then there’s the mysterious case of Chikungunya virus, which seems to trigger arthritis-like joint pain in women over age 40. LJI Assistant Professor Daniela Weiskopf, Ph.D., is investigating this strange phenomenon, which blurs the lines between infectious disease and autoimmune disease.
Learn more:
For some women, one mosquito bite leads to chronic pain
Pregnancy is an especially dangerous time to catch a viral infection. LJI Professor Sujan Shresta, Ph.D., is investigating how the mosquito-transmitted Zika virus thwarts the maternal immune system to breach the placenta and cause severe birth defects in the developing fetus.
In a recent study, Dr. Shresta’s lab uncovered a surprising way that Zika virus evades immune cells. Her research may guide the development of vaccines that boost helpful immune-cell responses to Zika virus and several other closely related viruses.
“Understanding how these viruses manipulate the immune response can help guide the development of the best vaccine approach,” says Dr. Shresta.
LJI Professor, President & CEO Erica Ollmann Saphire, Ph.D., MBA, is leading critical efforts to advance treatments for a hemorrhagic fever virus called Lassa virus. Lassa virus infection has around a 90 percent mortality rate in pregnant patients, making it a major threat to women in West Africa.
The Saphire Lab recently solved a mystery around how Lassa virus replicates itself within host cells. This discovery may lead to new therapies that interrupt this replication process, preventing severe infections. Dr. Saphire’s team has also shown exactly how a cocktail of three human antibodies can block viral infection. Scientists hope to test this antibody cocktail in future clinical trials.
When men and women get older
Some sex-based differences don’t rear their ugly heads until we get older. In a recent study, LJI William K. Bowes Distinguished Professor Pandurangan Vijayanand, M.D., Ph.D., and collaborators at the University of Southampton uncovered a specialized army of T cells with the power to trigger severe asthma attacks.
These T cells, called cytotoxic CD4+ tissue-resident memory T cells, are most commonly found in the lungs of men who develop asthma after age 40.
Dr. Vijayanand now hopes to learn more about cytotoxic CD4+ tissue-resident memory T cells—and their role in asthma development—as he works to advance more personalized therapies for asthma patients.
Speaking of T cells—we’ve long known that Parkinson’s disease is around twice as common in men as in women. But scientists weren’t able to explain the reason for this difference.
LJI Professor Alessandro Sette, Dr.Biol.Sci., has discovered that some people with Parkinson’s disease produce T cells that appear hell-bent on damaging healthy tissue. These “autoreactive” T cells are primed to charge into the brain and target dopamine-producing neurons, which are the same neurons that die off in Parkinson’s disease. Without dopamine-producing neurons, a person will develop the tell-tale tremors of Parkinson’s disease—and more severe symptoms as the disease progresses.
Dr. Sette’s laboratory recently investigated how T cells react to a protein called PINK1. PINK1 normally helps with brain-cell function, but the Sette Lab found that some people with Parkinson’s disease have T cells that mistakenly see PINK1 as a sign of disease. Those T cells may target brain cells that express PINK1, contributing to inflammation and the die-off of dopamine-producing neurons.
This T-cell activity was much more common in men. “The sex-based differences in T-cell responses were very, very striking,” says Sette. “This immune response may be a component of why we see a sex difference in Parkinson’s disease.”
Dr. Sette’s discovery could lead to tools that detect PINK1-targeting T cells as a biomarker of Parkinson’s disease, which may allow for earlier diagnosis. Scientists might even find ways to develop personalized therapies for Parkinson’s patients who show this harmful T-cell response.
The future of sex-based differences research
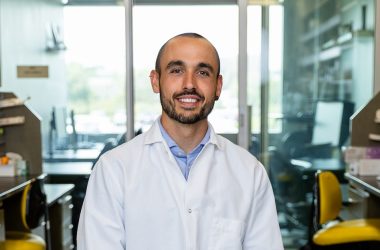
What’s next for LJI researchers? LJI Assistant Professor Miguel Reina-Campos, Ph.D., is harnessing a cutting-edge approach called “spatial transcriptomics” to study how immune cells mobilize to fight prostate cancer.
By tracking immune cells, Dr. Reina-Campos hopes to learn how reducing testosterone levels (the common treatment for prostate cancer) alters immune-cell function. Our immune cells can sense testosterone, after all.
Learn more:
T cells can sense testosterone—What does that mean for prostate cancer therapies?
LJI scientists are bringing us closer to a world where personalized medications and vaccines take sex-based differences into account. And their discoveries have sparked the curiosity of the wider public.
Over the past four years, Dr. Sharma has traveled the country to meet with experts from groups such as Women’s Health Access Matters (WHAM). She’s also spoken at industry convenings such as the 2025 Power of X Summit in New York, NY; members-only gatherings such as a BIGHORN community event in Palm Desert, CA; and with national audiences through virtual events such as LJI’s Live from the Lab webinar series, sponsored by the Global Autoimmune Institute.

Through these events, Sharma has found that more and more people are looking for ways to support the sex-based differences research pioneered by LJI scientists.
“We’re seeing critical energy coalescing around sex-based differences research,” says Dr. Sharma. “People are asking, ‘How can we do more?’”