“Vaccines are incredible,” says Shane Crotty, Ph.D., Professor and Chief Scientific Officer at La Jolla Institute for Immunology (LJI). “They are the only medicine recommended for every healthy person on the planet.”
Dr. Crotty and his colleagues recently launched the LJI Center for Vaccine Innovation. This center is home to researchers with the expertise to shape the future of vaccine design.
“LJI is one of the few places in the world that can measure all the different kinds of immune responses to a specific vaccine. We focus on the fundamental immunology of vaccines. Why does any vaccine work? And how can we get them to work better?” says Dr. Crotty. “The LJI Center for Vaccine Innovation will be the place that companies and other academic institutions come to understand their vaccine candidates.”
Speed is key
Just 19 years ago, Nepal had zero cases of dengue virus infection. Now the virus is endemic there. People in West Africa always thought they were safe from Ebola virus—until the virus began taking lives in Guinea in 2013.
Pathogens mutate. They travel the world. That’s why LJI scientists have developed tools to quickly assess immune cell responses and guide vaccine efforts against unexpected disease outbreaks.
In early 2020, Dr. Crotty and LJI Professor Alessandro Sette, Dr.Biol.Sci., published the very first study into how immune cells respond to COVID-19. They reported that human B cells and T cells could recognize and target SARS-CoV-2. This discovery gave scientists hope that a COVID-19 vaccine was possible. “We were able to rapidly hammer out some of the key questions,” says Dr. Sette.
The LJI team moved so quickly thanks in part to key infrastructure established at LJI back in 2003: the Immune Epitope Database (IEDB). This database, co-led by Dr. Sette and LJI Professor Bjoern Peters, Ph.D., includes tools to predict how human T cells can target pathogens.
The LJI Coronavirus Task Force went on to publish important research into immune cell responses to COVID-19 infections, different COVID-19 vaccines, and the ever-growing list of COVID-19 variants of concern.
Dr. Sette calls this series of SARS-CoV-2 breakthroughs the “poster child” that shows what LJI laboratories are capable of.
LJI scientists also formed new collaborations with laboratories around the world and shared data, computational tools, reagents, and laboratory supplies as they raced to beat COVID-19. “That was very powerful,” says LJI Research Assistant Professor Alba Grifoni, Ph.D., who co-led several pivotal COVID-19 studies. “We’re still thinking along those same lines when we hear about a disease outbreak. How can we come together to do something about it?”
Fight every virus
In 2020, Drs. Crotty, Sette, Grifoni, and LJI Research Assistant Professor Daniela Weiskopf, Ph.D., reported that many people already had T cells that recognized SARS-CoV-2, even if they had never been exposed to the virus before. These individuals had caught common cold coronaviruses in the past, so they had T cells primed to “cross-react” to SARS-CoV-2.
Normally, individual T cells and B cells are good at hunting down specific threats. A T cell that fights a Salmonella infection is trying to target that pathogen and nothing else, for example. “Cross-reactive” immune cells are special because they recognize features that different, though closely related, pathogens have in common.
“If we can provide broad protection at the level of T cells against different members of a viral family, then we could be very much ahead of the game,”
LJI Professor Alessandro Sette, Dr.Biol.Sci
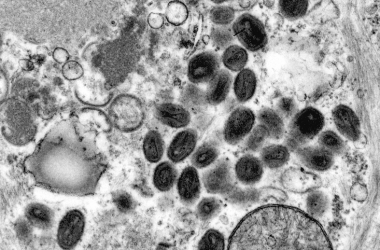
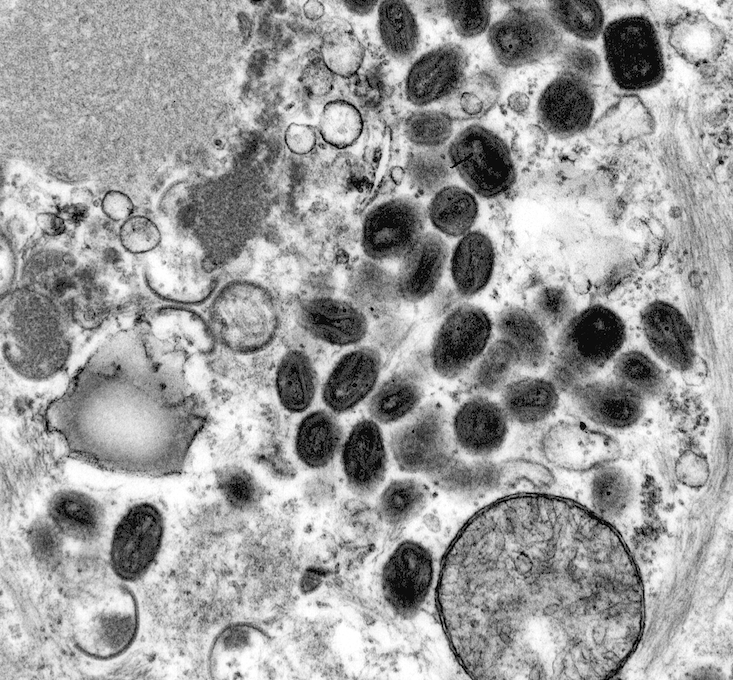
Drs. Sette and Grifoni are examining immune cell cross-reactivity as a way to develop new vaccines against a huge range of viruses with pandemic potential. Their laboratories are combining experimental findings with IEDB tools to predict how immune cells may react to viruses such as mpox, pertussis (whooping cough), Lassa virus, and SARS-CoV-2. Already, they’ve demonstrated that T cell cross reactivity gives the JYNNEOS mpox vaccine, which was developed to prevent smallpox, its fighting power.
Safe vaccines for all
LJI Professor Sujan Shresta, Ph.D., is one of the world’s leading experts on mouse models of viral infections. Her laboratory developed the first mouse models designed to help understand how T cells respond to flaviviruses such as dengue, Japanese encephalitis, Zika, West Nile, Powassan, and deer-tick. These viruses are carried by mosquitoes or ticks, and they are spreading rapidly around the globe, posing an ever-greater threat to human health, including in the continental United States.
Dr. Shresta’s ultimate goal is to develop pan-flavivirus vaccines—vaccines that protect against multiple flaviviruses at once. Different flaviviruses tend to co-circulate in the same geographic ranges and her work has already shown that flavivirus-cross-reactive T cells can protect against multiple diseases. Furthermore, Dr. Shestra’s mouse models make it easier to test how well flavivirus vaccines work and if they are safe.
“You need an animal model to study what is really happening in the immune system following infection or vaccination, and our mouse models provide that much needed tool to flavivirus researchers,” says Dr. Shresta.
Safety is indeed a huge concern for pan-flavivirus vaccine efforts. Dr. Shresta’s research was the first to show how flavivirus infections can trigger a phenomenon called “antibody-dependent enhancement,” where antibodies against one virus can leave the body vulnerable to other viruses. Fortunately, Dr. Shresta’s research suggests we can save lives by designing flavivirus vaccines that trigger strong T cell responses, rather than relying on antibodies.
Dr. Shresta is working on a vaccine candidate that does just that. Over the last decade, her laboratory has honed a “self-amplifying” RNA platform for vaccine production. With this kind of vaccine platform, scientists can design a vaccine that tells a patient’s cells to start making small pieces of a viral molecule. T cells then encounter these molecules and learn to recognize their structure.
“This could provide long-term protection,” says Dr. Shresta.
Dr. Weiskopf is also taking a close look at vaccine safety. She studies T cell responses to dengue virus, SARS-CoV-2, Chikungunya virus, and COVID-19 vaccines. For her dengue research, she’s working with doctors in the Philippines to regularly collect blood samples from children who received a dengue vaccine several years ago. This vaccine, developed by a pharmaceutical company, was quickly shelved after scientists found it could lead to more severe dengue cases in some patients.
Dr. Weiskopf is trying to figure out why it failed. Could it be related to antibody-dependent enhancement? Or something else? Vaccines are known for being safe and effective. The dengue vaccine was an exception, and Dr. Weiskopf wants to make sure it stays that way.
Longer-lasting vaccines
Dr. Weiskopf is also one of several LJI experts investigating exactly how long our immune cells “remember” past infections and vaccines. Vaccine durability is a big question in immunology right now, as health officials look to researchers for recommendations for how often a person should get COVID-19 vaccine “boosters.”
“We test immune responses in the blood a year after a person gets a vaccine, but what about after two years, three years, five years?” says Dr. Weiskopf. “We have a lot to learn about how to maintain an effective vaccine response.”
Dr. Crotty has uncovered new strategies to make vaccines work better and last longer. His laboratory focuses on B cells, which have the important job of churning out antibodies against specific pathogens. Dr. Crotty recently demonstrated that spreading out vaccine boosters can prompt B cells to make better and better antibodies to neutralize HIV, a virus notorious for evading human antibodies.
Vaccine ingredients make a difference, too. Most vaccines include a kind of adjuvant, a chemical that helps alert the immune system to danger and ramp up the immune response to the vaccine. For years, scientists have designed vaccines with an adjuvant called alum. Dr. Crotty’s work suggests new types of adjuvants can actually improve vaccine responses.
Capturing viruses in action
LJI Professor, President, and CEO Erica Ollmann Saphire, Ph.D., MBA, uses high-resolution imaging tools, such as cryo-electron microscopy, to map viral structures. Her team is one of the few in the world with the expertise to capture detailed, 3D images and videos showing how deadly viruses transform as they infect host cells.
Dr. Saphire’s three-dimensional maps are critical for vaccine design. Ebola virus, for example, uses a “glycoprotein” shield of sugar molecules to hide from the immune system. But Dr. Saphire’s team has shown there are fleeting moments in the Ebola virus life cycle where the glycoprotein structure shifts and human antibodies can swoop in to neutralize the virus.
These maps also show the areas where Ebola virus doesn’t mutate—the “load-bearing” pieces of viral architecture that stay the same over time. Like with cross-reactive T cells, human antibodies can recognize these “conserved” regions across related viral species. This research brings scientists closer to developing a pan-filovirus vaccine, which could protect people from Ebola virus, Sudan virus, Marburg virus, and other related viral species.
A place for vaccine breakthroughs
Vaccine research teaches us how immune cells work together and detect danger. This basic research is important for understanding how to better treat cancers, autoimmune diseases, heart disease, and much more. The LJI Center for Vaccine Innovation brings together the scientists who can make these connections. “We’ve got people who are really excited to collaborate,” says Dr. Crotty.
Dr. Crotty and his colleagues work closely with LJI’s world-class research cores. Experts in LJI’s Clinical Studies Core, Department of Laboratory Animal Care, Flow Cytometry Core, Next Generation Sequencing Core, and many other research services support vaccine innovation at the Institute.
“We’ve made amazing accomplishments and we’re excited to keep moving forward,” says Dr. Crotty. “We’re one of the best places in the world for solving problems in vaccine research.”
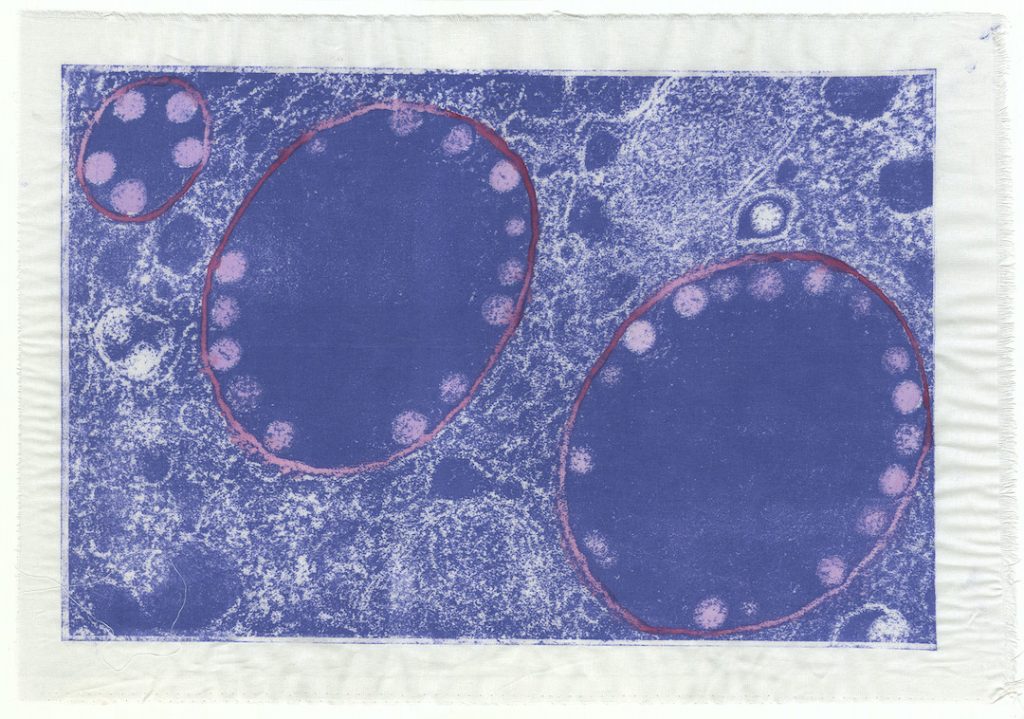
About the artist: Shannon Bodrogi is a mixed-media printmaker, originally from California, now living in Seattle, Wash. You can find their work at psiclopspress.com or follow them on Instagram @psiclopspress.