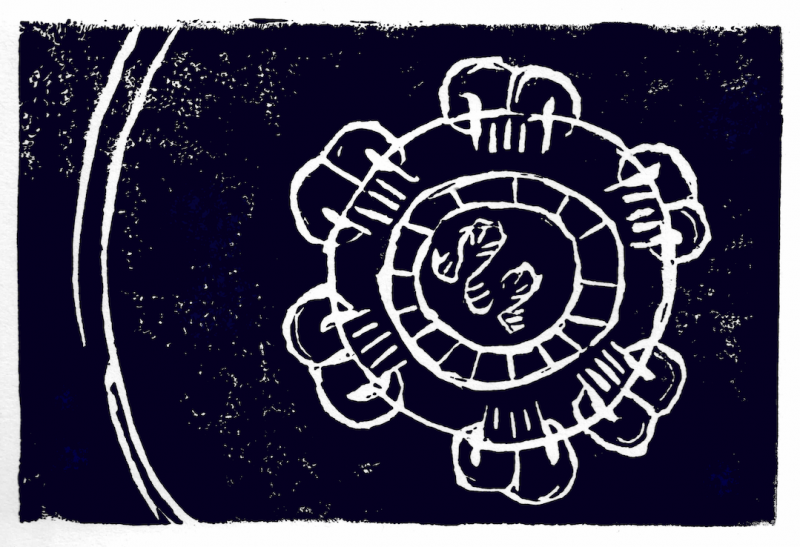
Dengue virus actually comes in four varieties, or serotypes. These serotypes are different enough that some researchers argue that they should be considered four separate viruses. Design a vaccine against one serotype, and you risk leaving someone vulnerable to the other three. Worse yet, due to a strange immune system phenomenon called antibody-dependent enhancement, a vaccine that works against only one or two serotypes can worsen a person’s response to the other serotypes.
These are big scientific challenges, but there’s more to the story.
“We don’t really have any safe and effective vaccines or antiviral therapies for dengue,” says La Jolla Institute for Immunology (LJI) Professor Sujan Shresta, Ph.D. “There are a lot of reasons for that. One of them is that dengue is a ‘disease of the poor.’ Until recently, it affected mostly low- to middle-income countries.”
Dr. Shresta is careful with her language. Researchers have devoted their careers to understanding dengue, and they’ve made progress. Still, dengue virus research remains poorly funded in many countries.
“We can’t continue to do science the way it’s been done,” says Dr. Shresta. “We need to have a more equitable relationship with developing countries. It’s actually a win-win situation, as robust infectious disease research can only happen in communities where viruses are actively circulating and evolving.”
Dr. Shresta grew up in Nepal and knew early on that she wanted to be an immunologist. She also saw how scientists in Nepal lacked the resources to tackle many public health issues. “I wanted to do something that would specifically help Nepal,” she says. “I think it’s really important for people from that part of the world to be involved in researching scientific problems that affect them and to share their findings with the rest of the world. This is also a good way to study emerging diseases before they become a pandemic and reach the United States.”
As she completed her scientific training, Dr. Shresta realized Nepal faced an emerging threat. “I had never heard of dengue,” she says. “This was 20 years ago but now it’s everywhere, including in the United States. Every decade, dengue is in more and more countries and there are more and more outbreaks.”
“We can’t continue to do science the way it’s been done… We need to have a more equitable relationship with developing countries.
LJI PROFESSOR SUJAN SHRESTA, PH.D.
Dr. Shresta watched the virus spread across the map as tropical Aedes mosquitoes moved into more temperate zones, bringing dengue virus with them. As she feared, warmer global temperatures soon gave the mosquitoes access to Nepal. “I wish we were wrong,” says Dr. Shresta. “But it was exactly as we predicted.” Today, more than half of the world’s population is at risk of dengue infection.
So Dr. Shresta set out to create a new tool to fight dengue: a very special mouse that can be infected by dengue as if it was a human. Scientists had been unsuccessfully trying to develop a mouse model of dengue virus infection for 50 years. Dr. Shresta designed relevant mouse models as a postdoctoral fellow at UC Berkeley.
“Today, we use these mouse models to tease apart the different cells involved in the immune response to these viruses,” says Dr. Shresta. “We can also tease apart what specific mutations or parts of the virus are doing—how they are interacting with the host.”
These models are important for studying new, urgent questions about dengue virus and its family: the flaviviruses, which also include Zika and Japanese encephalitis virus. “When Zika emerged in Brazil, we had a lot of questions. It wasn’t a new virus, but it was an obscure one,” says Dr. Shresta.
Like dengue, Zika had long been a disease limited to low- and middle-income countries. There were a lot of unknowns about how the immune system would recognize the virus. In particular, scientists needed to know how Zika would affect Brazilians already exposed to endemic dengue virus. [Read article: Fighting Zika? Call in the T cells]
“Zika and dengue are so closely related I feared there could be issues related to cross-reactive immune responses,” says Dr. Shresta. To answer these questions, she designed “sequential infection” experiments to infect mice with first dengue and then Zika, recreating the pattern seen in humans. Indeed, her results showed that the cross-reactive immune response to dengue and Zika can play both a good and bad role, and her laboratory is now studying how to harness the good and avoid bad aspects of this cross-reactive immune response.
The Shresta Lab’s mouse models are particularly useful for testing vaccine candidates and antivirals. This work helps scientists further refine vaccine and antiviral design. As of 2020, the FDA had only approved two antiviral drugs against dengue for clinical testing in humans, and in both cases the companies behind these drugs gathered safety and efficacy data using Dr. Shresta’s mouse models.
“Not many pharmaceutical companies have been interested in dengue,” says Dr. Shresta. “But, based on our data, these two companies got huge grants from the NIH to go forward and test these drugs in people.”
Dr. Shresta knows the way to help the most people is through a “pan-flavivirus” vaccine that protects against the four dengue serotypes and the closely related Zika virus. This kind of broad vaccine may also protect against the closely related Japanese encephalitis virus. The challenge is to get a vaccine to activate a strong immune response without triggering antibody-dependent enhancement.
“You have to have a balanced immune response from multiple perspectives—on the antibody side and the T-cell side—for these five different viruses. It’s a huge task,” says Dr. Shresta.
It’s a task she hasn’t been afraid to tackle head on. Since 2017, Dr. Shresta has been working closely with scientists at a San Diego biotech to help develop an RNA vaccine against these viruses. In 2020, her lab reported their RNA vaccine could protect against Zika in a mouse model. Dr. Shresta has since invested in the equipment to generate RNA and advance this work at LJI.
But her mind is never far from Nepal. Her lab has hosted researchers from Nepal, and several of Dr. Shresta’s lab colleagues have cross-trained with scientists in Nepal. In 2021, after 10 years spent building strong relationships with researchers overseas, Dr. Shresta received funding to study the spread of coronaviruses and flaviviruses in Nepal, Thailand, Vietnam, and the Philippines. [Read article: Building true partnerships with overseas labs]
This is the type of epidemiological research needed to study emerging infectious diseases, which do not care about borders, as COVID-19 has painfully demonstrated in the last few years.
As part of this NIAID-funded effort, Dr. Shresta is co-leading a Nepal research team with Professor Krishna Manandhar, Ph.D., of Tribhuvan University in Kathmandu, Nepal’s top research university. Dr. Shresta and Dr. Manandhar are working with scientists in Nepal to follow a large group of Nepalese volunteers and study how their immune systems react to coronavirus infections and flaviviruses, such as dengue virus.
After decades of trying and failing to stop the spread of dengue, this kind of true scientific partnership may fuel a new era of research.
Dr. Shresta hopes to prove that science and technology can be forces for economic development in Nepal—and she wants Nepalese researchers to be seen as leaders on the global stage.
Read more about Dr. Shresta’s research
Related video: What if immune “crosstalk” could make malaria partially protective against dengue fever?