Mosquitoes hide. They bite. They kill. One million people die from mosquito-borne illnesses every year. The mosquito is the deadliest animal in the world.
So how does the human body react when it meets a mosquito-borne virus? That’s a great question. “We know very little about the immunologic changes in the skin after a mosquito bites you,” says LJI Professor Sujan Shresta, Ph.D., an infectious disease researcher at La Jolla Institute for Immunology (LJI).
In fact, scientists face many big questions when it comes to the diseases spread by animals.
An estimated 80 percent of diseases are zoonotic, meaning they can be transmitted between humans and animals. Spillovers happen all the time. HIV came from other primates. MERS came from camels. “Zoonosis is everywhere. This is where pandemics come from,” says LJI Professor Erica Ollmann Saphire, Ph.D. “We are constantly interacting with birds and mammals and insects. There are rats in the subways and birds that leave waste in our water sources.”
The bubonic plague was a zoonotic disease. So was the 1918–1919 flu pandemic. And COVID-19. Monkeypox, potentially carried by rodents or other mammals, is the latest animal-borne threat.
Several LJI laboratories are dedicated to understanding how zoonotic diseases emerge—and how we can prevent them.

Flaviviruses
As a kid growing up in Nepal, Dr. Shresta wasn’t worried about dengue virus. The mountainous nation was too chilly for Aedes mosquitoes, which carry the virus. Then, as she trained as an immunologist, Dr. Shresta watched dengue march across Asia.
Today, dengue is endemic to Nepal, and Dr. Shresta is working closely with Nepalese research partners to understand the disease. She has devoted her career to studying how the immune system responds to dengue and other mosquito-borne flaviviruses, such as Zika and Japanese encephalitis virus.
“These diseases are major public health problems worldwide,” says Dr. Shresta. “Dengue and Zika affect half the world’s population. They are spreading in every tropical and subtropical country in the world.”
Through pioneering work in mouse models, Dr. Shresta has shown how the immune system responds when it encounters flaviviruses and how exposure to these viruses can harm developing fetuses.
Dr. Shresta is also interested in a phenomenon called “antibody-dependent enhancement,” or ADE. In ADE cases, subsequent infections by related viruses can accelerate, rather than blunt infection, leading to more severe disease. By studying ADE, Dr. Shresta is helping develop safe vaccines for people who live in areas where several flaviviruses overlap.
There’s no time to waste as climate change and warmer temperatures drive a global mosquito migration. In recent years, three species of Aedes mosquitoes were spotted in San Diego County for the first time.
Rabies virus
Humans have always feared rabies. Think vampires, werewolves. “This is an ancient disease,” says Dr. Saphire.
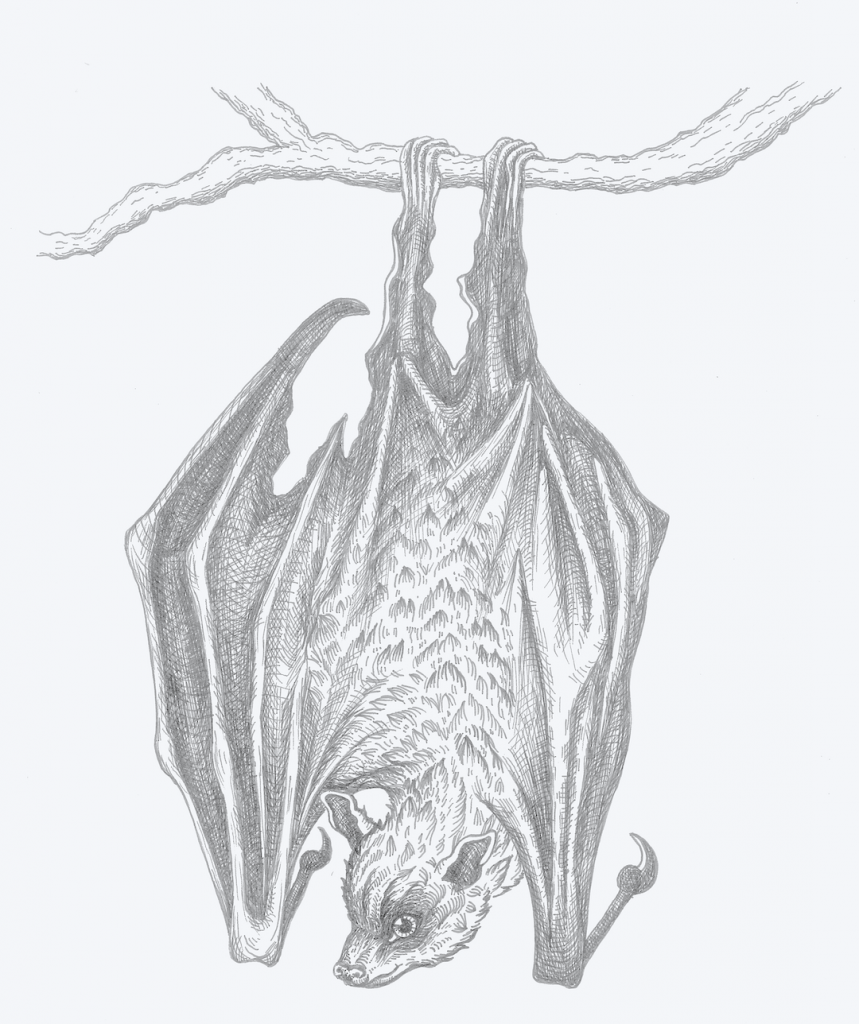
Rabies spreads between mammals through their bodily fluids, like saliva and blood. The virus is especially common in bats, raccoons, skunks, and foxes.
“Regardless of where you live in the United States, somewhere in your state is a creature that has rabies,” says LJI Postdoctoral Fellow Heather Callaway, Ph.D. “If you are exposed, you must get treatment or you will die, because rabies is 100 percent lethal if not treated.”
An estimated 59,000 people die from rabies each year. Most of the victims are children. Rabies treatments work, but they are inaccessible for most people around the world and unaffordable. (The treatment cost of $4,000 to $7,000 would devastate the average family).
Vaccines are a more realistic option—but they don’t last long enough. “Rabies vaccines don’t provide lifelong protection. You have to get your pets a booster shot every one to three years,” says Dr. Saphire.
To be frank: rabies vaccines are outdated. “The current rabies vaccines for humans and domesticated animals are made with killed or inactivated virus,” says Dr. Saphire. “These processes can spring the viral molecules into the wrong shape, so your immune system is distracted by the wrong thing.”
What rabies vaccine researchers have needed is a clear view of the rabies glycoprotein—a potential vaccine target on the viral surface. “It is important to understand that structure to make more effective vaccines and treatments—and to understand how rabies and other viruses like it enter cells,” says Dr. Saphire.
So Drs. Callaway and Saphire are using modern tools to solve an ancient problem. Thanks to advances in cryo-electron microscopy, they are capturing some of the first 3D images of the rabies glycoprotein, giving scientists the first glimpses of where the rabies virus might be vulnerable.
“Regardless of where you live in the United States, somewhere in your state is a creature that has rabies.”
HEather Calloway, Ph.D.
COVID-19
A coronavirus was likely circulating in an animal population (perhaps civet cats) when it mutated to spread from animal to human—and then from human to human. Who knows how many coronavirus variants circulated in the wild before the wrong animal made it to Wuhan, China.
Scientists refer to a virus-carrying animal population as a reservoir. Reservoirs are a problem because a large group of infected animals makes a fertile proving ground for dangerous viral mutations.
We’ve already seen how mutations can change SARS-CoV-2: human immune cells have a harder time fighting some SARS-CoV-2 variants, even in people who have been vaccinated.
To make matters worse, humans are hopping on planes and going on with their daily lives, seeding SARS-CoV-2 back among animal populations. “We’re the reservoir now,” says Dr. Saphire.
Already, SARS-CoV-2 has sickened mink, hamsters, tigers, and gorillas, among others. SARS-CoV-2 is now common in white-tailed deer in the Eastern United States. We’ve created reservoirs for SARS-CoV-2 in animals that posed no danger before.
Ebola virus
Dr. Saphire has witnessed the threat of animal reservoirs in her Ebola virus research. Time and time again, Ebola virus will appear in a community, seemingly out of nowhere. Then the outbreak will end and the disease will appear eradicated—until the virus reappears years or decades later.
Ebola virus can disappear and reappear because it can survive in an animal reservoir. Many studies point to fruit bats as the probable source. By persisting in an animal reservoir, Ebola virus can travel to new areas undetected. So far, Ebola virus has five cousins (that we know of), and they all pose a threat.
Dr. Saphire and her colleagues are eager to help design vaccines or therapies that fight all five ebolavirus species. By comparing the molecular structures of these viruses, the researchers can spot antibody targets the viruses have in common.
Engineering immunity
We don’t know which zoonotic disease will emerge next. No one expected monkeypox to spread so widely this year. LJI scientists want to be ready for anything. Their goal is to “engineer” immunity against specific viral targets—weak spots that a family of viruses may have in common.
“There are actually more than 70 known flaviviruses that could emerge and cause an explosive outbreak,” says Dr. Shresta. Her research suggests a pan-flavivirus approach is the best option.
Dr. Saphire, who is LJI’s President and Chief Executive Officer, leads the global Coronavirus Immunotherapy Consortium (CoVIC) and is working on a vaccine to tackle whichever coronavirus species emerges next. Dr. Shresta is a member of this consortium, and the two are collaborating to understand the best immunization strategies and key immune cells to activate with this kind of pan-coronavirus vaccine.
Meanwhile, Dr. Callaway has succeeded in capturing a clear 3D image of the rabies glycoprotein. Her recent work, published in Science Advances, may guide the development of better vaccines against rabies and the whole family of lyssaviruses.
These researchers are chipping away at the big questions—and they are making progress. Earlier this year, the Saphire Lab showed how a pair of antibodies can fight off Ebola virus and the closely related Sudan virus. This is a key step toward a pan-ebolavirus vaccine.
Doctors have a saying: “When you hear hoofbeats, think of horses, not zebras.” It means doctors should consider the most likely diagnoses first.
But LJI immunologists have to prepare for the most far-fetched possibilities. “We can’t play a game of whack-a-mole every time a virus emerges, where we shut down and try to make a vaccine against just that virus,” says Dr. Saphire.