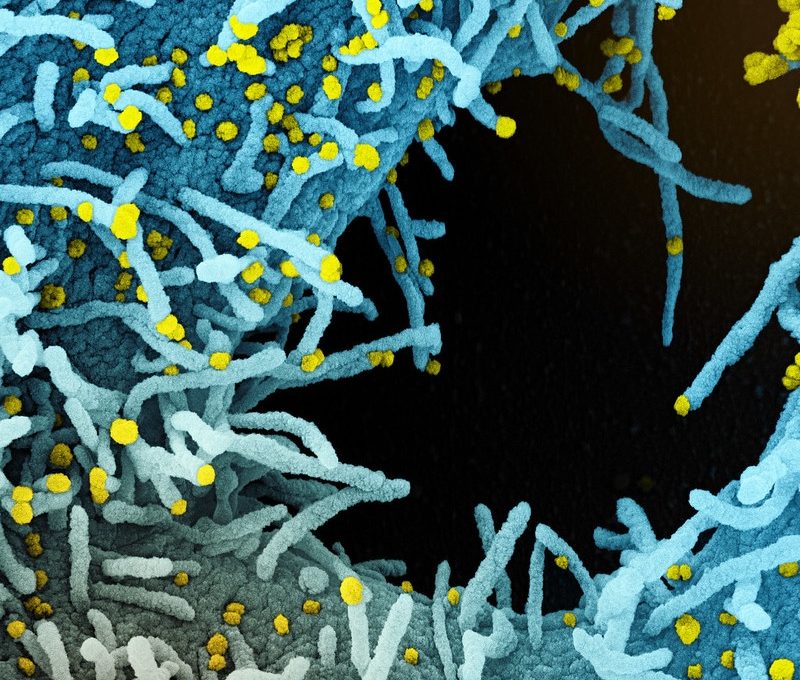
The closer we look, the more obvious it is that our immune cells and reproductive systems are bound together.
The clues have been there the whole time—ask anyone with a uterus.
We know that a bout of influenza or stomach flu can throw the menstrual cycle off by a few days. We know that seasonal allergies worsen at different stages of the menstrual cycle.
These phenomena are well supported by scientific research—and the discoveries just keep coming. Wondering whether a recent vaccination has shifted your menstrual cycle? Scientists have discovered that COVID-19 vaccination is indeed “associated with a small, temporary increase in menstrual cycle length.”
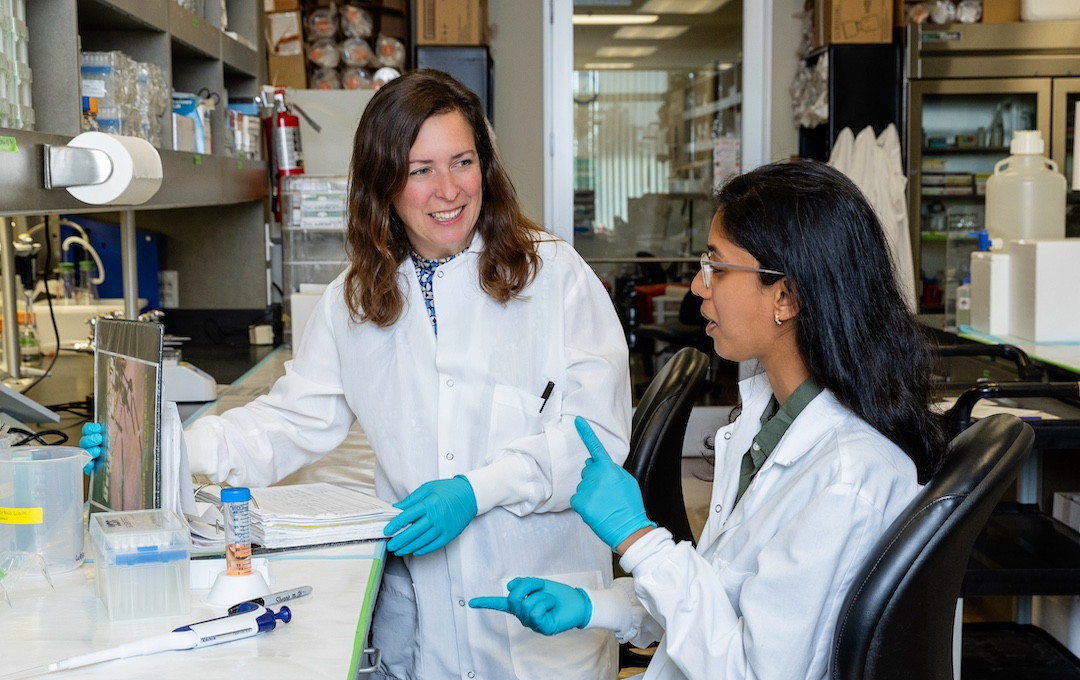
Researchers are still in the relatively early days of figuring out how sex-related differences, such as hormone levels, affect the immune system. At La Jolla Institute for Immunology (LJI), researchers Laura Hinojosa, a UC San Diego Graduate Student and member of LJI’s Ay Lab, and LJI Postdoctoral Fellow Amparo Martínez Pérez, Ph.D., who works in the Weiskopf Lab, are investigating some key questions.
Their goal is to shed light on basic biology—and open the door to new, more personalized medications for everyone.
How do hormones shape the immune system?
Hinojosa is addressing a major knowledge gap when it comes to oral hormonal contraceptives, also known as birth control pills. Her research has been a long time coming. The first hormonal contraceptive was approved by the U.S. Food and Drug Administration in 1957. Today, around 30 percent of women in the United States between the ages of 19 and 29 use hormonal contraceptives.
Yet we don’t know how these contraceptives affect immune function in people with XX chromosomes. “What surprises people is that even though hormonal contraceptives are very safe and they’ve been around for a long time, there are still a lot of questions we haven’t tackled,” says Hinojosa.
Hinojosa recently won $25,000 in funding from the Tullie Family Foundation through The Tullie and Rickey Families SPARK Awards for Innovations in Immunology to kick-start new research into these questions.
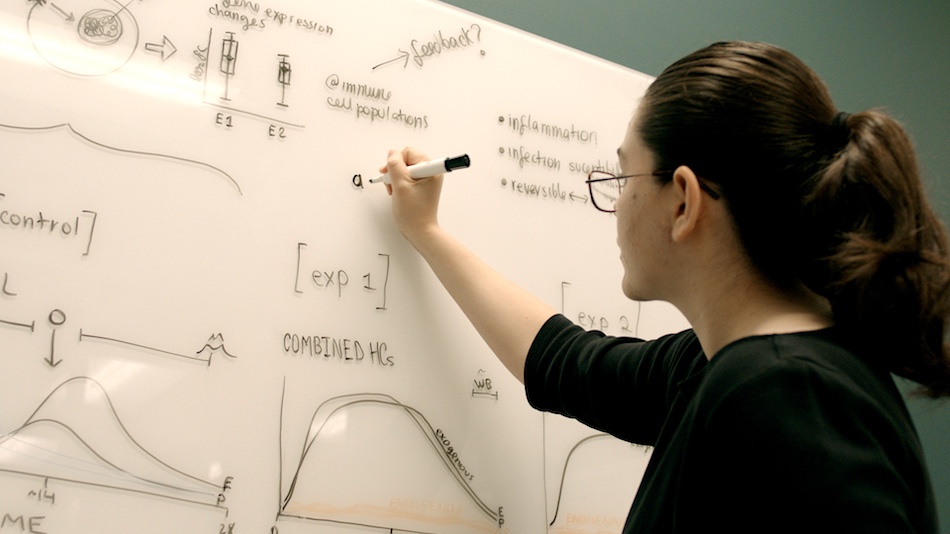
“I’m very interested in figuring out what’s going on, at a molecular level, when you take these contraceptives,” says Hinojosa.

Most of the cells in our immune system have the ability to respond to fluctuations in sex hormones, explains Hinojosa, so it makes sense that contraceptives would impact immune responses. We know about some of those impacts already. For example, researchers have found that using hormonal contraception affects a person’s risk of developing an autoimmune disease. At the same time, taking hormonal contraceptives appears to decrease the risk of developing certain conditions, such as severe asthma.
“Do hormonal contraceptives affect the immune system’s basal, or ‘resting,’ state?” asks Hinojosa. “Are we more prone to inflammation or not?”
Hinojosa will compare immune cells from volunteers who have never taken a hormonal contraceptive with those of volunteers who have taken either a progestin-only oral contraceptive or a combined estradiol and progestin contraceptive.
Hinojosa is getting ready to start recruiting clinical study participants, who will donate blood samples through LJI’s John and Susan Major Center for Clinical Investigation. She’s already heard from women who are interested in contributing.
“The most common comment I’ve had is from people telling me about their personal experiences with hormonal contraceptives, whether it’s been a good experience or an experience where they had an unexpected side effect,” says Hinojosa.
A new way to study endometriosis
Meanwhile, Dr. Martínez Pérez has won Tullie and Rickey Families SPARK Awards funding, provided by the Rosemary Kraemer Raitt Foundation Trust, to study a gynecological disease called endometriosis, which affects 1 in 10 women of reproductive age.
In this disease, the “endometrial” tissue that normally lines the uterus accidentally starts growing in areas such as the ovaries, fallopian tubes, and on the tissue that lines the pelvis. This endometrial tissue then thickens and breaks down with every menstrual cycle. The process leads to scar tissue and can leave organs stuck together.
No one is quite sure why endometriosis develops. We do know that endometriosis is an extraordinarily painful disease and a common cause of infertility.
“Understanding endometriosis would be a huge step forward for women’s health,” says Dr. Martínez Pérez.

Dr. Martínez Pérez wants to figure out how T cells behave in endometrial tissue. These cells survey the reproductive tract, looking for infected or cancerous cells. Could their malfunction be driving endometriosis? Dr. Martínez Pérez will study whether the T-cell population looks different in healthy people versus people with endometriosis.
Dr. Martínez Pérez will collect samples of monthly menstrual blood and analyze the T cells from both healthy volunteers and volunteers with endometriosis. She’s eager to learn whether T cells from volunteers with endometriosis may react to certain markers in endometrial tissue and drive inflammation.
The collection method is wonderfully straightforward: menstrual cups. Many people routinely use flexible, silicone menstrual cups to manage bleeding during menstruation. Why not collect that blood for science?
“This collection method has been done before, but you still don’t find many research papers about lymphocytes in the menstrual blood, even though they are one of the most abundant immune populations there,” says Dr. Martínez Pérez.
Dr. Martínez Pérez would be the first to use menstrual cups to collect samples at LJI. She’s working now to prepare the study protocol and volunteer resources.
Dr. Martínez Pérez believes volunteers will step up to donate their menstrual blood to aid endometriosis research. “The feedback on this project has been great,” she says. “Even people without endometriosis have come up to me and said they want to participate.”
“I hope to continue this research as I go further in my career,” adds Dr. Martínez Pérez. “I would love to be dedicated to understanding women’s health and immunology.”
Learn more:
LJI Center for Sex-based Differences in the Immune System
The Tullie and Rickey Families SPARK Awards for Innovations in Immunology