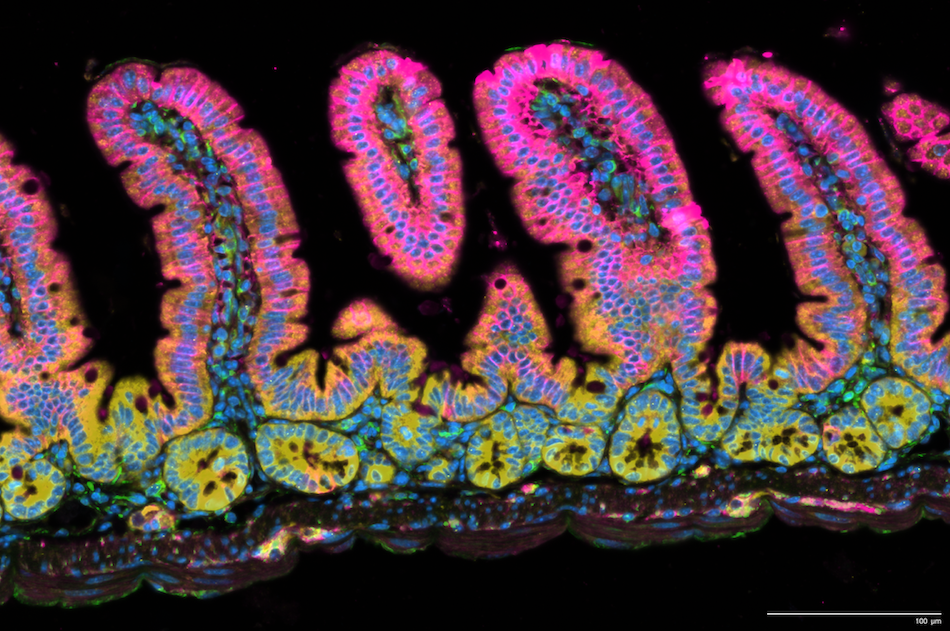
The future is bright for prostate cancer research. It’s glowing, in fact, thanks to new tools that combine the eye-catching fluorescence of microscopy with next-generation sequencing tools.
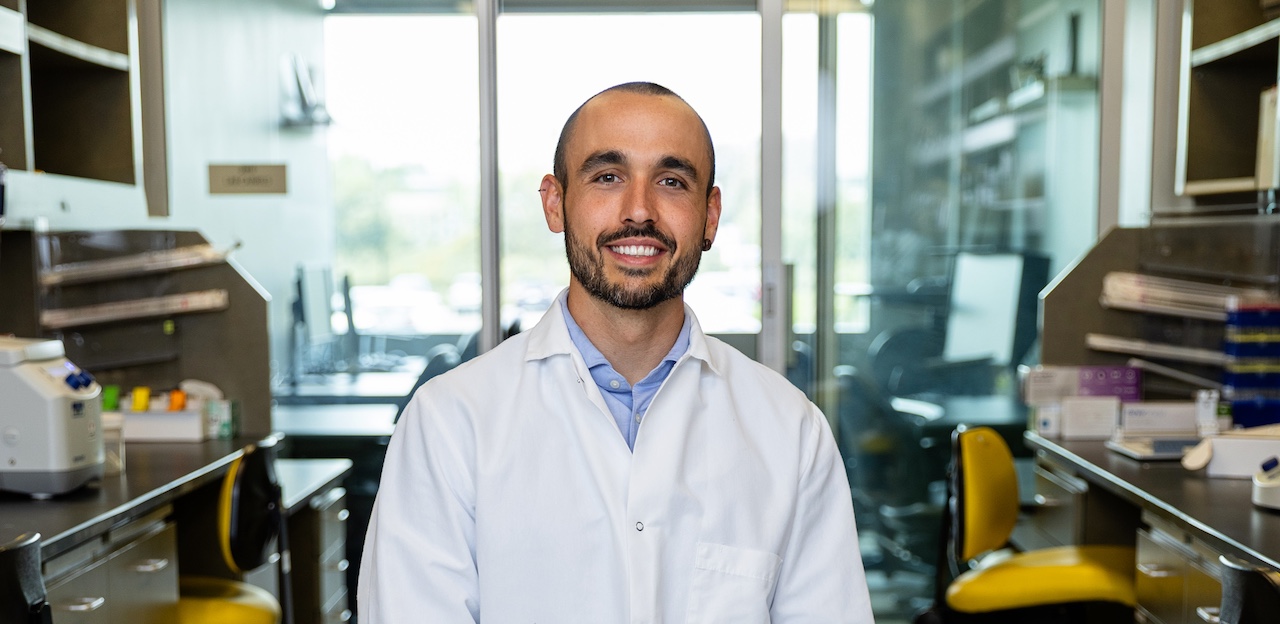
LJI Assistant Professor Miguel Reina-Campos, Ph.D., specializes in using spatial transcriptomics tools to advance the field of tissue immunology. Spatial transcriptomics gives scientists a way to track where immune cells are located (the “spatial” part) and exactly how those immune cells are trying to protect the body (the “transcriptomics” part).
By tracking this immune-cell activity, Dr. Reina-Campos can help guide the development of new immunotherapies for prostate cancer, a disease that kills around 35,700 men each year.
“No one has ever profiled tissues like this before,” says Dr. Reina-Campos. “Spatial transcriptomics enables us to look at hundreds of thousands of cells and thousands of genes in prostate tissues.”
When you take away testosterone
Already, Dr. Reina-Campos has shown the power of spatial transcriptomics in studying T cells that fight pathogens in the gut. He has also developed a promising approach for powering up T cells to better fight tumors.
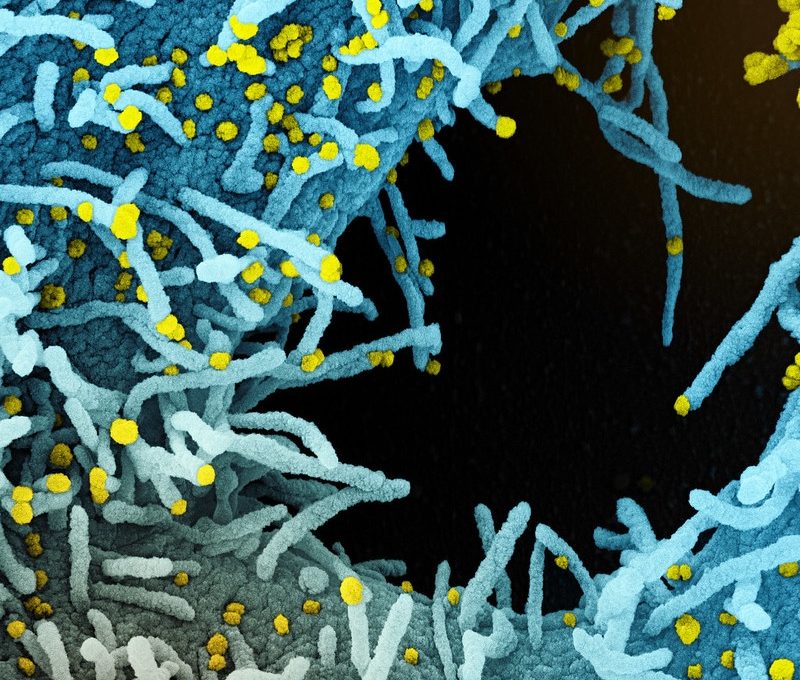
Now Dr. Reina-Campos is investigating how specialized “tissue-resident memory CD8+ T cells” fight prostate cancer.
Scientists know these T cells have the power to kill tumor cells. But T cells don’t work alone. They interact with other immune cells, and they can sense a huge range of signaling molecules, including testosterone and estrogen. These signaling molecules direct T-cell activity, including antitumor activity.
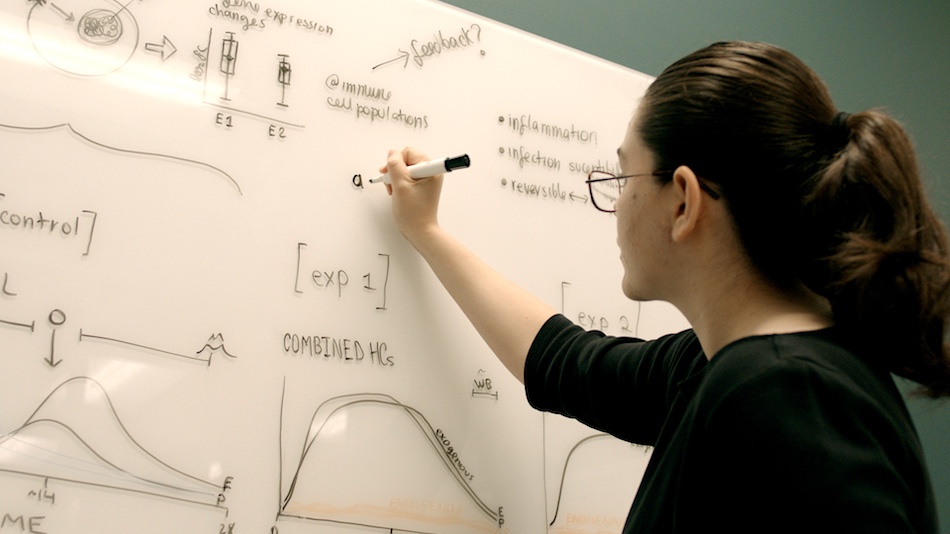
So what happens if you need to fight a tumor, but you suddenly take away testosterone?
“The standard of care for prostate cancer is androgen deprivation—or ‘chemical castration’—in which you reduce testosterone levels almost to zero,” says Dr. Reina-Campos. “But the role of testosterone and its sensor, which is an androgen receptor on immune cells, is not really well known.”
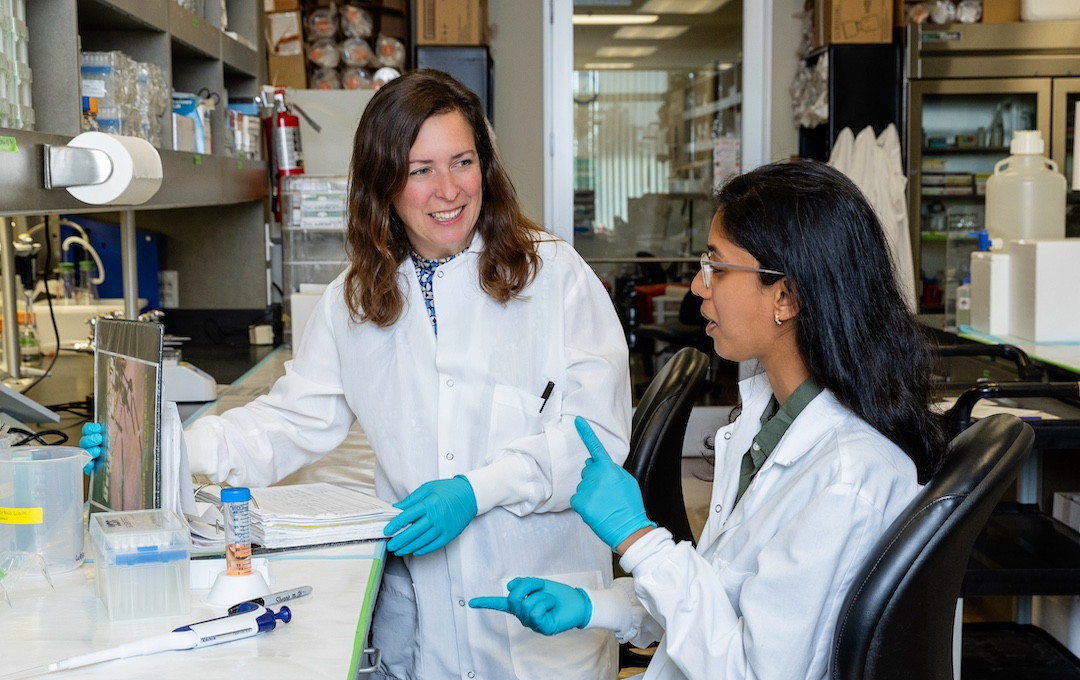
Scientists need to know how androgen deprivation affects cancer-fighting T cells. With spatial transcriptomics, Dr. Reina-Campos can track T-cell activity before and after androgen deprivation. He can uncover exactly which kinds of T cells jump into action and how those T cells travel through tissues to find their targets.

Prostate cancer research may be just the beginning. Dr. Reina-Campos is looking forward to working closely with collaborators, here in San Diego and across the country, to understand how skyrocketing estrogen levels during pregnancy affect T-cell activity in mammary tissue.
Dr. Reina-Campos is also contributing to UC San Diego and Salk Institute studies into how immune cells guard the placenta to stop disease at what scientists call the maternal-fetal interface.
“This research follows T-cell function all through the monthly cycle, all the way through pregnancy and giving birth—which is when hormone levels really change,” says Dr. Reina-Campos. “This is part of trying to understand the underlying mechanisms of the immune system.”
With spatial transcriptomics, Dr. Reina-Campos can track how T cells move, like glowing constellations, through our tissues. This is a new kind of cartography, a mission that may guide us toward better medicine for all.