In 2021, a team of researchers from South Africa analyzed data from 423,117 COVID-19 patients around the world.
Their study revealed a puzzling trend. Men were 46 percent more likely to be admitted to the ICU due to COVID-19 complications and 45 percent more likely to die from COVID-19 complications than women.
This sex-based difference has shown up in study after study, in country after country. There has been a lot of speculation about why this is. Perhaps men wait too long to seek medical care. Perhaps men are more likely to experience lung damage from smoking. Perhaps men are more prone to obesity and cardiovascular disease.
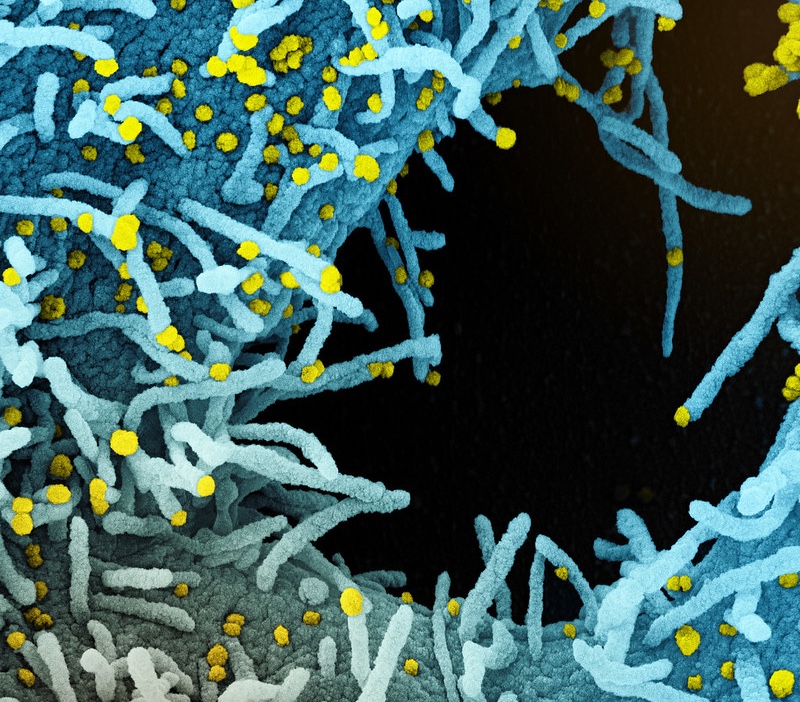
But when researchers controlled for lifestyle factors and co-morbidities, they still saw a difference in how men responded to SARS-CoV-2, the virus that causes COVID-19.
Four years ago, scientists had a lot of questions about why COVID-19 affected men and women differently. Now they have answers.
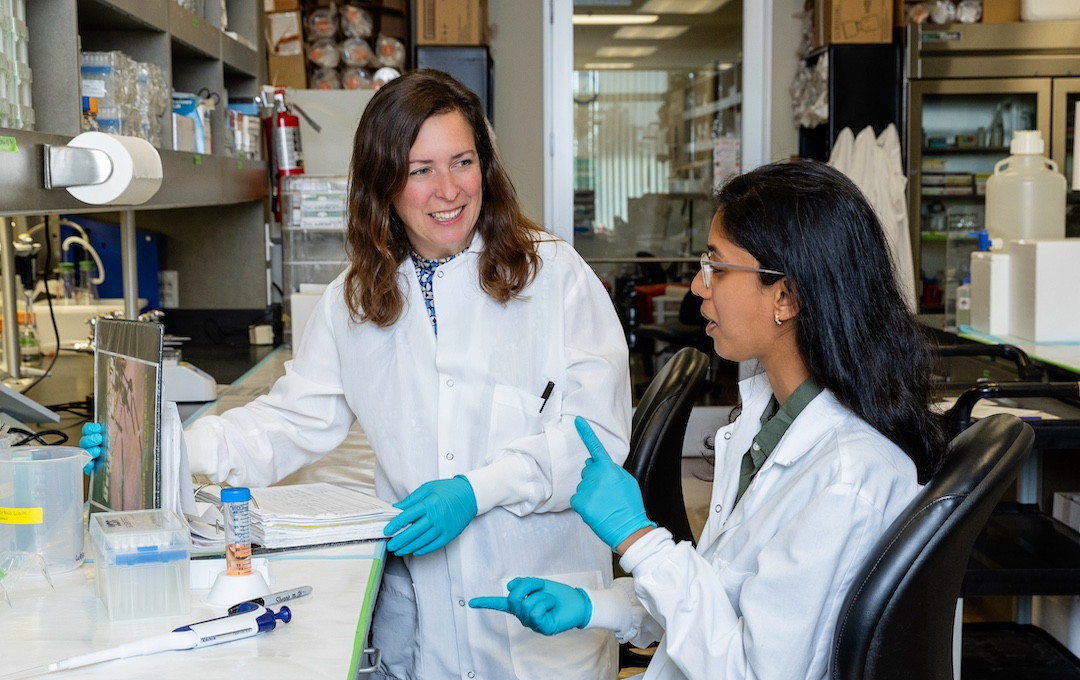
LJI Associate Professor Sonia Sharma, Ph.D., has discovered a fascinating sex-based difference in samples from the blood and respiratory tracts of male and female COVID-19 patients. In addition to the different virus-fighting cells and molecules in these samples, the study participants had varying levels of an enzyme called adenosine deaminase 2 (ADA2).
How a little enzyme makes a big difference
Immune cells churn out specific proteins for specific jobs. Many proteins are involved in cellular metabolism, a series of chemical reactions organized into the specific metabolic pathways that provide our cells and tissues with metabolites—where we get our energy and the building blocks of life.
Some metabolites also regulate the activation and function of immune cells.
ADA2 is a protein that removes a class of metabolites called purines, which stimulate immune cells.
Purines activate genetic sequences called human endogenous retroviral elements (HERV). Immunologists are interested in HERVs because these little RNA strands kick off the process of preparing cells in the innate immune system to fight pathogens. Without HERVs, your innate immune cells—cells such as macrophages, monocytes, and neutrophils—can’t combat viruses or alert other types of immune cells (such as T cells) to danger.
The immune system is strong, so the body has built-in ways to keep our powerful immune cells in check. ADA2’s job is to inhibit HERV expression, which tells innate immune cells to stand down when they aren’t needed.
Because of this, ADA2 is a great enzyme to keep around—in fact, patients who lack ADA2 develop an inflammatory disease called vasculitis. However, everything changes when a virus shows up.
The male COVID-19 patients in Dr. Sharma’s study had a problem. They produced a lot more ADA2 than the female patients.

“The first thing we noticed immediately were the sex-based differences,” says Dr. Sharma, who also serves as Director of LJI’s Center for Sex-Based Differences in the Immune System.
The differences were stark. With their higher ADA2 levels, it seemed the men had inhibited HERV expression. Without HERV expression, the male patients had a weaker antiviral immune response.
Dr. Sharma then analyzed a completely different group of COVID-19 patients. Again, male patients had higher ADA2 levels and lower HERV expression compared with female patients.
This sex-based difference held true even in healthy study participants. Healthy men had higher ADA2 levels compared with healthy women. Meanwhile, women taking estrogen-containing birth control showed the lowest levels of ADA2. As a result, the women had higher HERV expression.
Dr. Sharma thinks high HERV expression helps to “prime” innate immune cells in women, better preparing them to fight viral threats.
“This study illustrates a metabolic mechanism that causes differences between the antiviral immune response of men and women,” says Dr. Sharma. “This is a new mechanism behind immune responses, and we can show the consequences of differential metabolism and gene expression in men and women.”
Genes and consequences
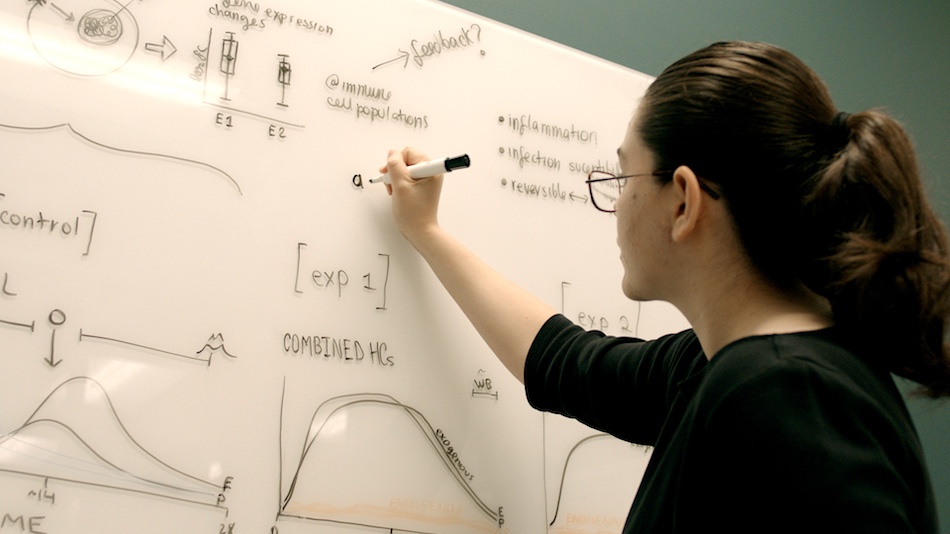
“Differential expression” is the key phrase here.
Some genetic differences are obvious. Men usually have a Y chromosome, and women usually have a second X chromosome. These sex chromosomes can influence how your immune cells work.
But sex chromosomes are just a small piece of a person’s genetic makeup. Aside from the two sex chromosomes, men and women have basically the same genes on their other 44 chromosomes. LJI scientists are interested in those cases in which male and female immune cells express different genes from this genetic toolbox.
LJI Research Assistant Professor Benjamin Schmeidel, Ph.D., and LJI William K. Bowes Distinguished Professor Pandurangan Vijayanand, M.D., Ph.D., have led the development of an LJI-hosted resource called DICE (Database of Immune Cell Expression, Expression quantitative trait loci [eQTLs] and Epigenomics), where scientists can compare gene expression in different immune cell types—and compare differential expression in men and women.
By harnessing DICE, Drs. Schmeidel and Vijayanand have shown that the male and female immune systems express wildly different genes—even when their immune cells have the same goal (such as fighting infection). They’ve found that the gene for ADA2 shows this differential expression.
Dr. Sharma’s new COVID-19 research demonstrates how this sex-based difference may affect actual disease outcomes.
Next steps: How do hormones change the game?
Dr. Sharma’s findings could also prove important for understanding men’s responses to many other acute infections.
Men carry higher a viral load when infected with hepatitis C or HIV, for example. Men also experienced significantly higher mortality during the Middle East Respiratory Coronavirus outbreak of 2012 (52 percent of men died, compared with 23 percent of women). This pattern was also seen in the SARS (Severe Acute Respiratory Coronavirus 1) outbreak of 2003 (in which 22 percent of men died, as opposed to 13 percent of women).
Many of these discrepancies may come down to small differences in gene expression between male and female immune cells.
Now, Dr. Sharma is especially interested in understanding how sex hormones affect certain molecules that trigger ADA2 expression.
“It really looks like sex hormones are driving some of these differences,” says Dr. Sharma. “From an evolutionary point of view, it makes sense that females would need more baseline protection against viral infections because they are having children—and they have to be healthy overall to do that.”