Your bile duct network is a true tree of life.
A floppy, pink tree of life.
The branches, smooth like spaghetti noodles, reach up to collect bile and waste from your gallbladder and liver. Farther down, the thick tree trunk—your common bile duct—joins with a pipeline from your pancreas. This whole system then empties into your small intestine.
Without a healthy bile duct network, the body cannot remove bile and waste products, and a person gets really sick, really fast. That’s why bile duct obstructions (usually from gallstones) so often require surgery.
Here’s the weird thing. Bile ducts ought to work exactly the same in every person, regardless of their sex. Yet women are far more likely than men to be diagnosed with a devastating autoimmune disease called primary biliary cholangitis (PBC).
“PBC is more common in women versus men. In fact, some studies have highlighted a 10-to-1 ratio,” says Job Rocha, a researcher at La Jolla Institute for Immunology (LJI) and UC San Diego Graduate Student. “For every male with PBC, 10 women have it. That’s a really dramatic difference.”
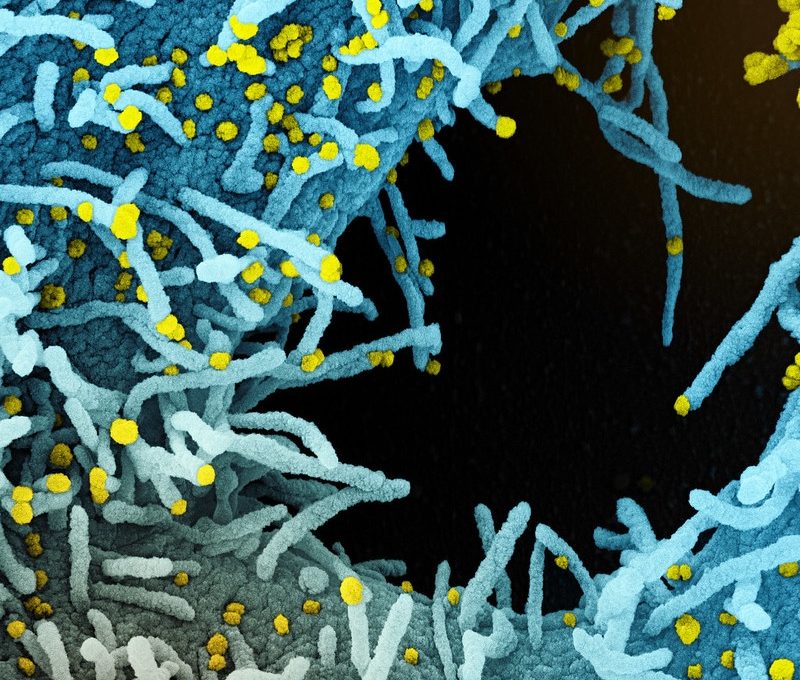
PBC develops when the immune system’s T cells mistakenly attack a person’s own bile ducts. The disease is chronic and extremely painful, and it can lead to end-stage liver cirrhosis.
Rocha wants to know why T cells make this mistake in the first place—and why PBC is so much more common in women. He was recently awarded the 2025 BioLegend Graduate Fellowship in Immunology to support his work. “This fellowship is a great honor,” says Rocha. “It means a lot for my career as a scientist, and it means my research can move forward.”
Asking the right questions
Rocha might be the perfect person to study what goes wrong in PBC.
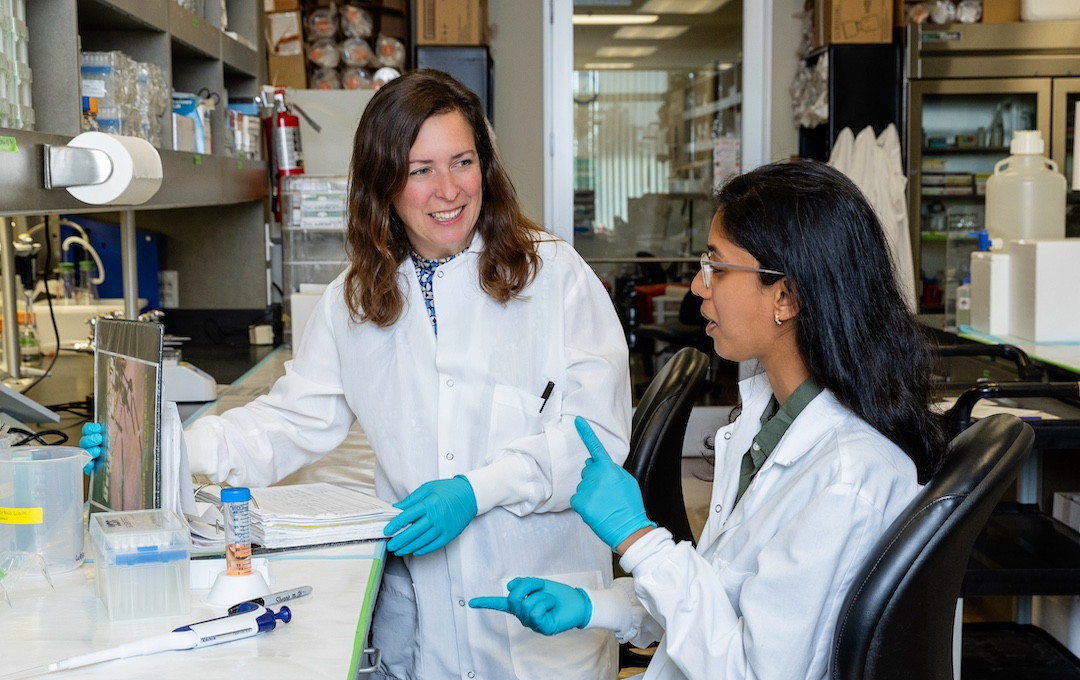
As a UC San Diego Graduate Student, Rocha is working in the labs of three LJI co-mentors: LJI Professor Hilde Cheroutre, Ph.D.; LJI Professor and President Emeritus Mitchell Kronenberg, Ph.D.; and LJI William K. Bowes Distinguished Professor Pandurangan Vijayanand, M.D., Ph.D. These mentors specialize in understanding T-cell biology, autoimmunity, and gene expression. Thanks to their guidance, Rocha has gained the expertise to zoom in and see how certain kinds of T cells may drive PBC development.
Rocha is especially interested in the role of T cells called mucosal-associated invariant T (MAIT) cells. MAIT cells make up 10–40 percent of immune cells in a healthy liver. “There are also studies showing MAIT cells around the liver, near the bile ducts,” says Rocha.
MAIT cells are good fighters. Researchers have found that MAIT cells can respond very quickly to infections. Their speed makes them invaluable when fighting pathogens, but in people with an autoimmune disease, MAIT cells may cause a lot of harm.
Rocha is investigating whether PBC might be linked to “friendly fire” from nearby MAIT cells. “Are these MAIT cells pathogenic or protective?” asks Rocha. “If they are pathogenic, then maybe we can think about how to deplete these cells in the future to slow down disease progression.”

Rocha is looking for clues among the “tissue-resident” immune cells that spend their time in the liver. For this research, Rocha has partnered with Professor Andy Mason, MBBS, FRCPI, of the University of Alberta, to analyze immune cells from human liver tissue samples. Rocha hopes to figure out whether this cell population, including the MAIT cells, differs between PBC patients and healthy controls.
Rocha is also searching for clues in the thymus, a small organ that sits beneath the sternum. The thymus is where T cells first develop (and where they get the “T” in their name.) Rocha is working with Dr. Cheroutre and Dr. Vijayanand to study MAIT cells and other specialized T cells found in human thymus samples, which were collected by collaborators at Rady Children’s Hospital.
The bigger mystery of autoimmune disease
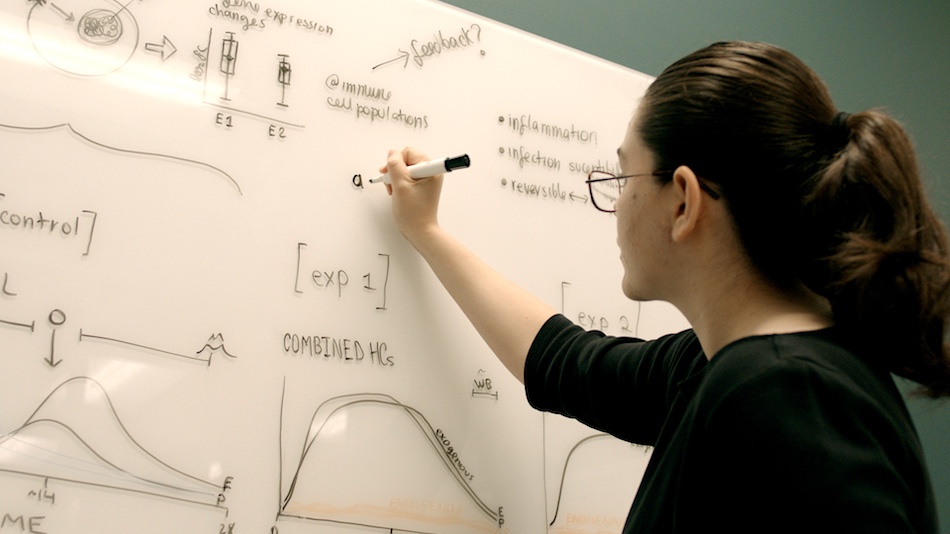
Piece by piece, Rocha is assembling a picture of how MAIT cells work—and the role of these cells near the bile duct network. His ultimate goal is to help scientists develop more effective therapies for PBC.
“The approved treatments don’t work for everyone,” says Rocha.
And that’s just for people who know they have PBC.
As Rocha explains, many people with PBC show some initial symptoms but aren’t diagnosed until years later—once they’ve developed end-stage liver disease. “The disease can go silent for 10 or 20 years after the initial onset of symptoms,” says Rocha. “Then, when you start to see symptoms again, it can be too late.”
Does this sound familiar? PBC isn’t the only autoimmune disease in which symptoms may fade in and out. Patients with multiple sclerosis and myasthenia gravis can even go into “remission” for stretches of time.
Studying PBC may give us a valuable window into how T cells behave in many types of autoimmune disease. Like PBC, almost all autoimmune diseases are more common in people with XX chromosomes. Multiple sclerosis, myasthenia gravis, rheumatoid arthritis, lupus, and Sjögren’s syndrome are just some of these.
Dr. Kronenberg is eager to see whether Rocha’s experiments with a mouse model of PBC will lead to answers. “We have mouse models here that reproduce a lot of features of the disease, including a higher prevalence in females,” says Dr. Kronenberg.
“We are hoping to understand what drives PBC, of course, but it would be really nice if we also had insight into a different biliary disease or a different autoimmune disease that shows similar features,” adds Rocha.
The bile duct network is so much more than a piece of plumbing. Teasing apart this delicate system may be key to understanding sex-based differences in autoimmune disease.