Scientists at La Jolla Institute for Immunology (LJI) are working to cure all disease through the power of fundamental research. Digging deep into specific immune cells, LJI scientists reveal the hidden genes and molecules that keep us healthy.
This approach has proven transformative since the Institute’s founding in 1988. Over the decades, scientists here have made groundbreaking discoveries across the spectrum of human health. LJI researchers have discovered key genes that drive cancer-fighting immune cells. They’ve uncovered how immune cells combat deadly pathogens. LJI labs have demystified autoimmune diseases, such as type 1 diabetes, and found clues about the immune system’s role in Parkinson’s disease.
Through their commitment to understanding the fundamental workings of immunity, LJI researchers have advanced medical science around the world and delivered hope to patients and their families.
“From our labs here in La Jolla, we punch way above our weight on the international stage. About 30 percent of our faculty are in the top 1 percent of scientists in their field,” says LJI Professor, President & CEO Erica Ollmann Saphire, Ph.D.
It takes time, and big investments, to turn fundamental scientific discoveries into new drugs and therapies to help patients. LJI Professor and Director of Academic Affairs Michael Croft, Ph.D., knows that journey well.
“It’s gratifying to see the work that you do as a fundamental immunologist—as a basic scientist—translated into human therapy,” says Dr. Croft.
Dr. Croft joined the LJI faculty in 1996. Just a few years later, he proposed something that had never been tried before.
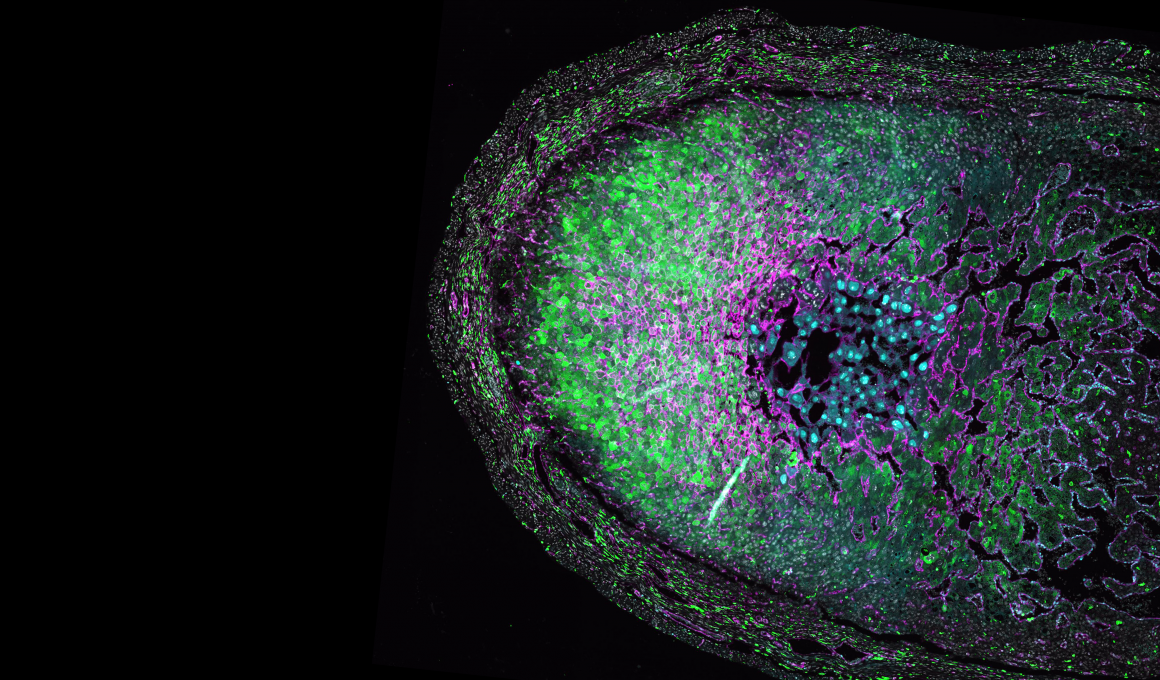
Dr. Croft’s lab was investigating a molecule expressed by immune cells, called OX40. They had discovered that OX40 activity could drive harmful inflammation and fuel dangerous allergic conditions, such as asthma and atopic dermatitis (the most common form of eczema).
So, Dr. Croft approached Kyowa Kirin Co., Ltd., a longtime research partner of LJI, with the idea to treat harmful inflammation by using antibodies to block OX40 activity. Scientists at Kyowa Kirin understood the importance of Dr. Croft’s proposal. They worked closely with Dr. Croft as they undertook an antibody discovery program. This resulted in an antibody, KHK4083, now termed rocatinlimab, an investigational T cell rebalancing therapy that targets the OX40 receptor expressed on the surface of pathogenic T cells.
Kyowa Kirin, along with their partner Amgen Inc., is now conducting clinical trials to evaluate the long-term safety and efficacy of rocatinlimab in several immune-mediated diseases, including in adults and adolescents with moderate-to-severe atopic dermatitis.
Bringing rocatinlimab to this stage has taken decades, and Dr. Croft has been there every step of the way, making fundamental discoveries that may lead to new treatment approaches for patients.
The spark of an idea

Dr. Croft trained as an immunologist during the 1980s. This was a decade of big discoveries as new technologies made it possible to track down many key genes and molecules that enable our cells to fight disease.
By the late 1980s, scientists in San Diego were leading pioneering research into cytokines, a group of “messenger” molecules made by immune cells. Our T cells and other immune cells use special receptor proteins to sense cytokines and act on those messages.
Dr. Croft was fascinated by cytokines. The immune system is extremely complicated. There are more than 100 immune cell subtypes, and each cell subtype has a different job.
If you could decode cytokine messages, you might reveal how the whole system worked.
“I thought this was an area where, potentially, you could find molecules that might be instrumental in driving the activity of T cells in any situation,” says Dr. Croft. “Whether it was T cells that were protecting against infectious diseases or cancer—or T cells that were driving autoimmunity.”
Milestones in fundamental science
One particular group of cytokines caught Dr. Croft’s eye: tumor necrosis factor (TNF) superfamily molecules. In 1996, Dr. Croft joined the LJI faculty and dedicated his lab to understanding TNF superfamily molecules and the T cell receptors that sense them.
Dr. Croft was especially interested in a TNF superfamily molecule called OX40 and its binding partner, OX40L. Dr. Croft’s lab was the first to show that these molecules tell T cells to multiply quickly when they sense a potential threat. OX40 and OX40L also allow T cells to survive in the body for a long time and promote T cell “memory.”
Dr. Croft also found that OX40 helps T cells remember allergens, so that when they sense an allergen again, they will multiply and release a flood of inflammatory cytokines. This inflammation ramps up quickly, blocking airways and sometimes causing an asthma attack or damaging skin tissues in a dermatitis flare-up.
That’s when Dr. Croft made his proposal. “The data we generated in those first few years after joining LJI suggested OX40 could be a terrific target for therapy,” says Dr. Croft.
Crafting a new kind of medicine

Dr. Croft’s insights and proposal led to Kyowa Kirin’s development of rocatinlimab, a monoclonal antibody therapy that blocks OX40-driven T cell responses. This intervention “rebalances” damaging T cell responses and dials back harmful inflammation.
“Our work with Dr. Croft over the years has been incredibly collaborative and supportive,” says Rachel Soloff, Ph.D., Kyowa Kirin’s Executive Director, Global Medical Affairs, Immunology. “Dr. Croft has been available to discuss the biology of OX40 and helped us understand how the OX40 pathway drives pathogenesis in inflammatory diseases.”
By investigating “messenger” molecules and the fundamental workings of immune cells, Dr. Croft has sparked an entirely new field of medical research. In addition to Kyowa Kirin, several pharmaceutical companies are currently conducting clinical trials to test antibodies to OX40 or OX40L to treat inflammatory diseases such as asthma, prurigo nodularis, alopecia areata, hidradenitis suppurativa, and celiac disease.
Now Dr. Croft is starting a new chapter himself. He will retire at the end of 2025, after 29 years on the LJI faculty. But he’s not going far. He will continue to serve as an advisor and mentor for many early-career researchers and junior faculty at LJI. Dr. Croft has seen how fundamental science can lead to real change for patients, and he hopes to help other researchers follow that path.
“You need patience to be a research scientist,” says Dr. Croft. “Results don’t come quickly. Results take a little bit of luck, as well as good knowledge, good planning, and good science.
A closer look at rocatinlimab
In March 2025, Kyowa Kirin and their partner in the development of rocatinlimab, Amgen Inc., released new top-line Phase III clinical trial data. The novel antibody approach led to statistically significant improvements for adult patients with moderate-to-severe atopic dermatitis (ROCKET-Ignite). This study showed statistically significant improvements in the Eczema Area and Severity Index (EASI) and validated Investigator Global Assessment (vIGA) response.
References: https://clinicaltrials.gov/study/NCT05398445 and https://bit.ly/3U0XB9V