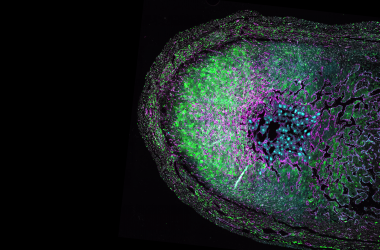
For years, many scientists thought of the brain as “immunologically privileged.” Few microbes can penetrate the brain, thanks to a layer of cells called the blood-brain barrier. This barrier also stops some immune cells and antibodies. In their place, specialized immune cells called microglia and astrocytes patrol the brain for danger.
It’s comforting to imagine the all-powerful brain cloistered away in the skull, bathed in a special immune cell soup.
Yet many diseases do strike the brain. Aggressive tumors, such as glioblastomas, aren’t shy about growing there. Alzheimer’s disease and Parkinson’s disease damage brain cells and steal memories. The wider nervous system isn’t safe either. Viruses can camp out in the nervous system for years, and many autoimmune diseases exclusively target nerves.
To stop these diseases, scientists at La Jolla Institute for Immunology (LJI) have embraced the growing field of “neuroimmunology.” By taking a closer look at how pathogens, immune cells, and the nervous system interact, these scientists have shown the brain is far from isolated.
The weird viruses that live in your nervous system

LJI Professor Chris Benedict, Ph.D., is interested in how viruses infect the nervous system—and why the body often fails to fight back. His laboratory focuses on a type of herpesvirus called cytomegalovirus (CMV). An estimated 70 percent of the population has CMV, and nearly 100 percent of the population has a similar herpesvirus called Epstein-Barr virus (EBV).
“This is a family of DNA viruses that once you’re infected with them, you’re infected for life. Your immune system can’t clear them,” says Dr. Benedict.
Dr. Benedict’s work has shed light on how these viruses evade the immune system. Using mouse models and next generation sequencing tools, he has shown that herpesviruses actually produce proteins that look very similar to human proteins. Immune cells try to fight back, but herpesviruses use these clever doppelgangers to trick the immune system into a cease fire. “They’re able to throw up these smokescreens and thwart your immune system,” says Dr. Benedict.
Once the initial battle is over, certain types of herpesviruses move into the nervous system, only occasionally reactivating to cause a rash or canker sore (depending on the type of herpesvirus). CMV doesn’t usually haunt the nervous system in adults. Instead, herpesviruses HSV-1 and HSV-2 are the lurkers.
At least that’s the case in healthy people. A fetus can get CMV too, and this kind of infection in utero is the leading cause of congenital deafness. Even a latent CMV infection can turn dangerous in someone with a weak immune system—as seen in cases where CMV reactivates in someone with AIDS. “When your immune system is suppressed, all of these herpesviruses come out of hiding,” Dr. Benedict explains.
“When your immune system is suppressed, all of these herpesviruses come out of hiding.”
LJI Professor Chris Benedict, Ph.D.
These are the rare cases where scientists know CMV is to blame. Because so many people have CMV and virtually everyone has EBV, it’s often hard to know whether a herpesvirus is driving a neurological disease or if it’s just along for the ride.
A 2022 study in Science showed a connection between EBV infection and the development of multiple sclerosis. Some studies have linked CMV to chronic fatigue syndrome. Cancer researchers studying brain tumors called glioblastomas have detected the CMV genome within the tumors.
“CMV is associated with glioblastoma, but most likely infection of the tumor cells (or tumor stem cells) happens at a very early stage in the womb (congenital infection). But does that mean cytomegalovirus is driving glioblastoma?” asks Dr. Benedict. “It’s always been a sort of a chicken-and-egg argument. Are these viruses causative or are they associative?
Dr. Benedict suspects these viruses are part of the cause in cases where someone is already genetically predisposed to a disease. Herpesviruses are, after all, experts at manipulating human cells. “A person might have a gene linked to a higher susceptibility for getting a disease such as multiple sclerosis,” he says. “Then EBV might further sensitize them for developing that disease.”
Secret messages from your brain
Dr. von Herrath is very interested in how the brain talks to immune cells. “The central nervous system controls the whole body, right?” says Dr. von Herrath. “So why wouldn’t the nervous system set the inflammatory immune ‘tone’ in certain organs?”
Tracking messages from the brain to the pancreas is key to Dr. von Herrath’s work to understand the origins of type 1 diabetes. Researchers know that type 1 diabetes occurs when self-reactive T cells start attacking the insulin-producing beta cells in the pancreas. In a 2020 study, Dr. von Herrath showed that everyone—not just people with type 1 diabetes—has these potentially harmful T cells. These T cells linger near the beta cells but don’t attack until they get some kind of signal. Dr. von Herrath thinks this signal may be coming from the nervous system.
Using mouse models, his laboratory has shown that blocking nerve signals to the pancreas can stop the onset of type 1 diabetes.
One clue that Dr. von Herrath is on the right track is that beta cells in the pancreas tend to die off in patches that correspond to the presence of nerves in the pancreas. He suspects the nervous system may be communicating with immune cells called macrophages, since macrophages have the right kinds of molecular receptors to receive certain signals from the nervous system.
“Figuring out whether the nervous system regulates immune function is really a new frontier,” says Dr. von Herrath.
Genetic sequencing guides the way

Sometimes the brain itself gets sick. Thanks to advances in neuroimmunology, LJI researchers are closer to understanding why.
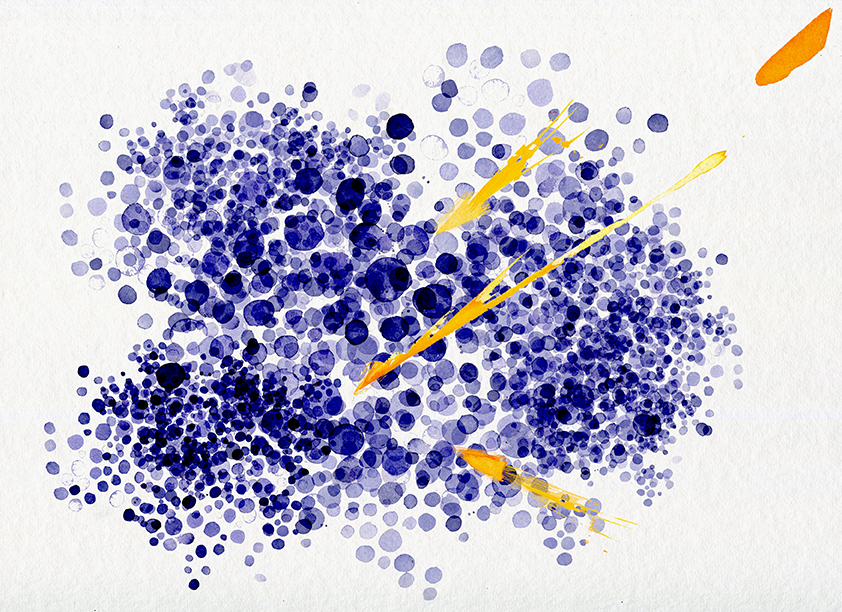
In a series of pivotal studies, LJI Professor Alessandro Sette, Dr.Biol.Sci., and Research Assistant Professor Cecilia Lindestam Arlehamn, Ph.D., have shown a clear connection between harmful T cells and Parkinson’s disease. In a collaboration with partners at Columbia University Irving Medical Center, the LJI team showed that dangerous, “self-reactive” T cells can be found in the brains of people with Parkinson’s disease.
These T cells are most active at the onset of Parkinson’s disease, and they are on a mission to find and attack misfolded alpha-synuclein proteins. Unfortunately, these misfolded proteins are found on dopamine-producing neurons—the very cells that die as Parkinson’s disease progresses.
Are self-reactive T cells to blame?
There’s still a lot to learn about these cells, but there’s mounting evidence that Parkinson’s disease onset may be an autoimmune process.
In a 2022 study in the journal npj Parkinson’s Disease, Drs. Sette and Lindestam Arlehamn showed that the T cells involved in Parkinson’s can express LRRK2, a gene associated with the genetic, or familial, type of Parkinson’s disease.
This gene expression had never been seen in T cells before—and the surprises continued. Many of the genes expressed in these T cells were completely unexpected and not previously linked to Parkinson’s disease. “This finding suggests we found novel targets for potential therapeutics,” says Dr. Sette.
Dr. Benedict says recent advances in genetic sequencing are key to connecting the dots between many more diseases and the nervous system. Across the Institute, many LJI laboratories are harnessing deep sequencing tools to understand how different genes are expressed in different types of immune cells. This research gives scientists a window into how the body fights—or surrenders to—different pathogens or diseases.
Just last year, Dr. Benedict collaborated with Dr. Sette to uncover exactly how T cells respond to CMV infection—work critical for future CMV vaccine design. Dr. Benedict has also partnered with LJI Professor Pandurangan “Vijay” Vijayanand, M.D., Ph.D., to use deep sequencing methods to tease apart the interplay of viral and immune cell gene expression.
“We are getting closer to understanding how genetics add to a person’s susceptibility to these diseases,” says Dr. Benedict. “That’s really the cutting edge.”
Original art by Ann Kiernan