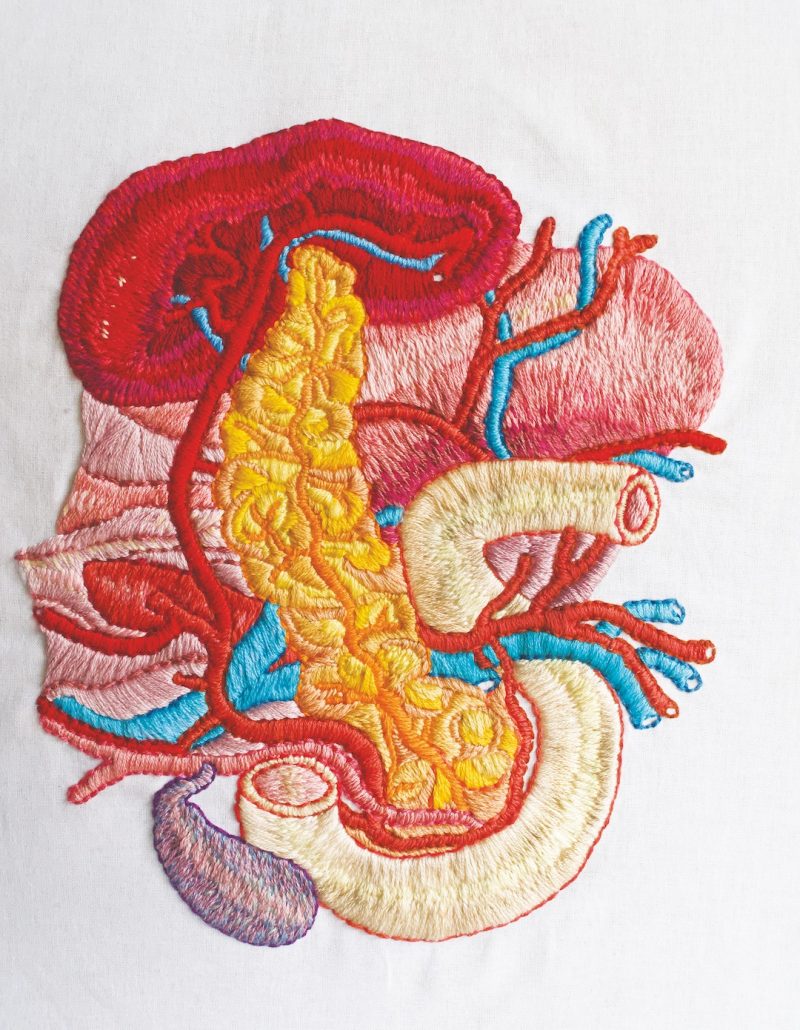
It’s easy to overlook the pancreas. It doesn’t have the beautiful symmetry of the brain or the muscular curves of the heart. Instead, the pinkish-yellow pancreas is shaped a bit like a squashed sweet potato.
Yet, the pancreas is a hidden gem.
From its perch behind the stomach, the pancreas spends its days churning out the life-giving enzymes that break down the sugars, fats, and starches in your food. Zooming in, small cell clusters called islets come into view. Special beta cells live nestled within the islets, busily making the insulin the body uses to regulate blood sugar.
Unless there’s trouble—with a capital T.
The body’s own T cells target and destroy these beta cells in people with type 1 diabetes. Without beta cells, blood sugar levels go haywire. Blood thickens, causing strokes, heart disease, blindness, kidney damage, even death.
No one knows what causes these “autoreactive” T cells to attack, but researchers at La Jolla Institute for Immunology (LJI) have uncovered some fascinating clues.
In a recent study, LJI Professor Matthias von Herrath, M.D., and LJI Postdoctoral Researcher Christine Bender, Ph.D., tracked the movements of T cells that attack beta cells. These T cells find the beta cells by targeting preproinsulin, the precursor molecule to insulin.
To their surprise, the researchers discovered these T cells gather in the pancreas in nearly everyone, not just people with type 1 diabetes. Then the T cells wait. The T cells should move into the islets like hyenas, but for some reason, they can’t see their prey until some unknown event forces the islets or beta cells to “unmask” themselves.
“These cells, which are supposed to be the bad guys, are actually present in healthy people,” says Dr. Bender. “They are already there, and then in type 1 diabetes, something triggers them to recognize the islets or the beta cells and attack them—and destroy them.”
“There has to be a component where the beta cells play an active role in revealing themselves to the immune system,” adds Dr. von Herrath.
With a watchful eye on these predatory cells, Dr. von Herrath is tracking down what triggers them to attack the beta cells. In a recent collaboration with Gustaf Christoffersson, Ph.D., a former LJI postdoctoral researcher, Dr. von Herrath exposed a possible culprit: nerves.
Using a mouse model of type 1 diabetes, the researchers found that beta cells die off in patches that match up with where the cells are “innervated,” meaning sensitized by nerves that branch out to the pancreas. The team found that blocking the nerve signals protected mice from beta cell death. “If the innervation is not occurring—like if you cut the nerves—then the organ remains invisible,” says Dr. von Herrath.
This discovery has led Dr. von Herrath to consider nerves as the triggers for other organ-specific autoimmune diseases. He points out that other autoimmune diseases show patterns of patchy cell death that may be linked to innervation.
One example is vitiligo, a skin condition in which pigment-producing cells die off, leading to pale areas of skin. These pale areas often show up around the mouth and hands in symmetrical patterns that may reflect the symmetry of the underlying nerves.
“Organs are innervated—the skin is innervated—and it might just be that the innervation of a given target organ or area plays a role in sensitizing that organ for immune destruction or unmasking,” says Dr. von Herrath. “If we could understand that, we could treat these diseases by modulating the nerves, which would be really cool.”
We’re in the early days of understanding the role of innervation in type 1 diabetes. Meanwhile, Dr. Bender is still on the hunt for T cells that may attack other targets on beta cells. The researchers hope that by finding the most vulnerable targets, they might be able to block specific T cell attacks and treat type 1 diabetes. Their goal is to protect the pancreas without affecting how the immune system does its job overall.
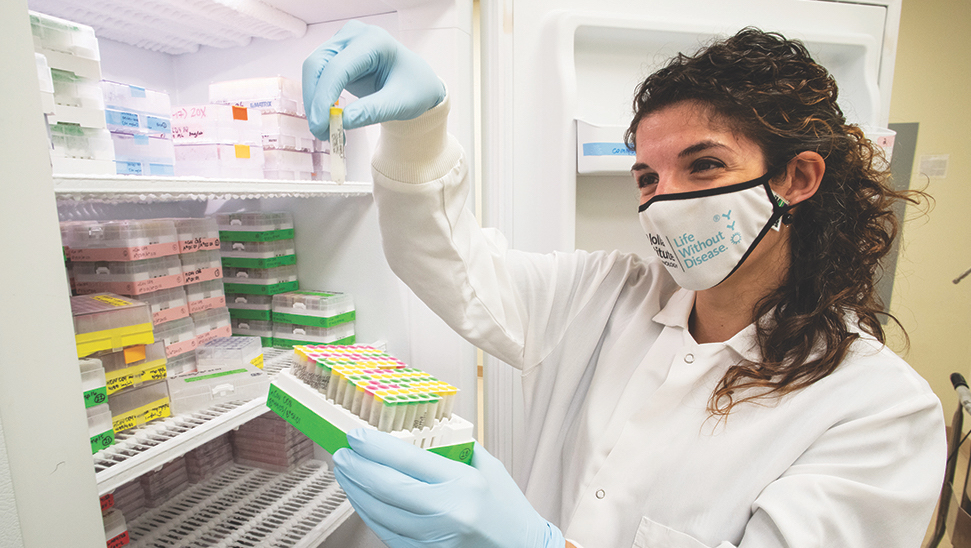
To do this, Dr. Bender is working with scientists in the LJI Microscopy Core to track how T cells move around the organ. “We can scan whole tissue sections to see the bigger picture,” says Dr. Bender.
The researchers are also working closely with tissue biobanks, making them one of the few teams with access to rare human pancreas samples. This is important because—while mouse models are very helpful—the islets of a human pancreas have a different architecture than a mouse pancreas.
“Having these human pancreas samples is unique,” Dr. Bender says. “The window they provide into the inner workings of the pancreas gives LJI researchers another powerful tool in understanding this critically important organ.”
The pancreas, that precious organ.
Local artist spotlight: The pancreas embroidery above by by San Diego-based artist and educator Patricia Pauchnick.